Translate this page into:
Post phacoemulsification shine: Iatrogenic foreign body deposition

*Corresponding author: Obaidur Rehman, Department of Oculoplasty and Ocular Oncology, Dr. Shroff ’s Charity Eye Hospital, New Delhi, India. obaid.rehmann@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Luthra A, Rehman O. Post phacoemulsification shine: Iatrogenic foreign body deposition. Lat Am J Ophthalmol. doi: 10.25259/LAJO_22_2024
Abstract
A 55-year-old woman, with a history of phacoemulsification and intraocular lens (IOL) implantation in both eyes, presented for a routine check-up. Slit-lamp examination of the left eye revealed a patch of silver-colored deposits with a metallic sheen at the 2 o’ clock iris position, absent on the conjunctiva or cornea, differentiating this from typical ocular argyrosis. The likely diagnosis was residual phacoemulsification tip deposits consolidated on the iris, an unusual post-surgical manifestation.
Keywords
Intraocular foreign body
Foreign body
Phacoemulsification
INTRODUCTION
One of the leading causes of avoidable blindness in the world is age-related cataractous changes in the lens, which is most commonly tackled using a Phaco-emulsification procedure. Phaco-emulsification basically consists of a Piezo-electric tip which oscillates at a frequency between 27 to 60 kHz, leading to nuclear piece emulsification, combined with simultaneous aspiration of the emulsified material. Phaco tips, usually made of titanium alloys, are available in different materials, sizes, and shapes. Long-term usage of the same phaco tip leads to increased roughness & brittleness, along with decreased efficacy of emulsification.[1] We present a rarely-reported complication of likely phaco tip fragment deposition.
DISCUSSION
A 55-year-old female with a recent history of uncomplicated phacoemulsification and IOL implantation in the left eye presented for a routine postoperative check-up. Visual acuity was 20/20, and the cornea was clear. Slit-lamp examination revealed a foreign body deposit with a metallic sheen at the 2 o’ clock iris position [Figure 1]. There was no history of recent trauma. The deposits were absent on the conjunctiva and cornea. The anterior chamber (AC) was quiet, with no signs of infection or inflammation. This finding was not noted pre-operatively and likely represented residual phacoemulsification tip metallic deposits consolidated on the iris, an unusual post-surgical finding. The patient has been on regular follow-up for the past 5 months, with no ocular complaints. Vision is maintained at 20/20 with clear cornea and quiet AC.
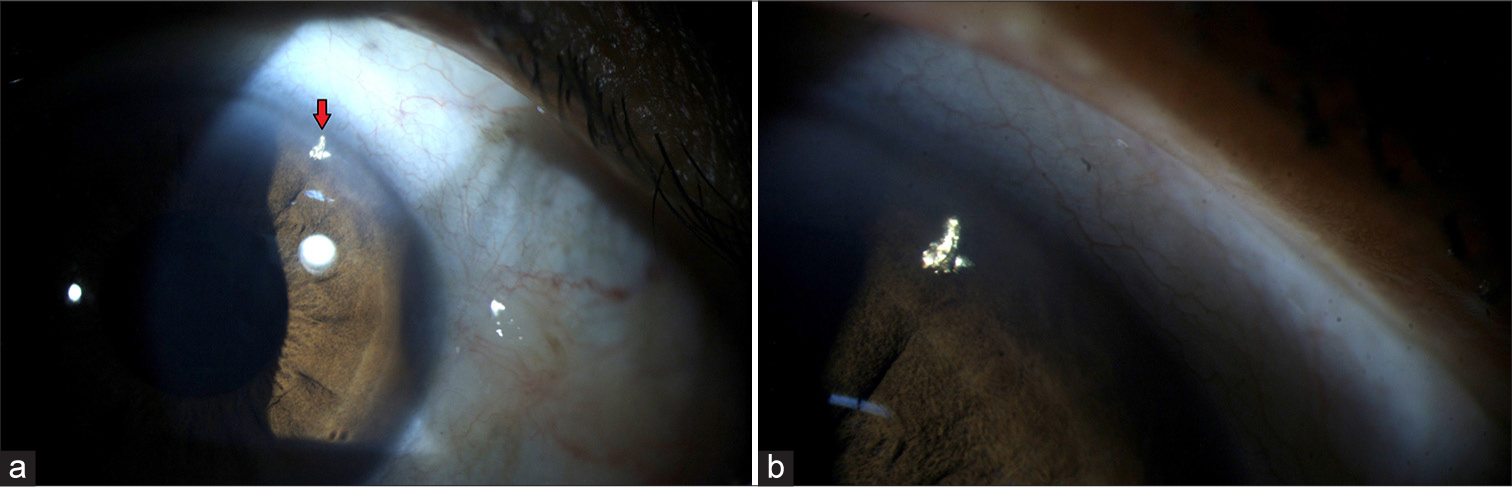
- (a) Red arrow mark showing the metallic foreign body deposition at 2 o-clock position; and (b) magnified image showing the foreign body deposition.
The anterior chamber is a common site for deposition of foreign body after cataract surgery. Post-phacoemulsification intraocular metallic foreign bodies, though rare, have been reported before.[2-4] The plausible causes are contact between the fast-oscillating Phaco tip and the Sinskey hook/chopper used during surgery, or the gradual cavitational erosion of the phaco tip.
The discovery of an inert foreign body in the AC is usually by serendipity. Depending on the nature of foreign body, the clinical presentation, and the surgeon’s experience, management may be conservative or surgical (foreign body removal).
CONCLUSION
Inert foreign bodies such as Titanium (in our case) may be left in situ, when sitting quietly. However, regular follow-up should be maintained to evaluate for signs of inflation/infection. Phacoemulsification, though one of the most performed surgeries world-wide, does not have well established guidelines as to the repeated usage of the same instruments in multiple surgeries and the ideal time for changing instruments, especially keeping in mind low socioeconomic status set-ups. There is a strong need to investigate factors which increase chances of instrument degradation and fracture, and arrive at a suitable guideline as to when instruments need replacement.
Ethical approval:
The Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship:
Nil.
References
- The Impact of Reused Phaco Tip on Outcomes of Phacoemulsification Surgery. Curr Eye Res. 2016;41:636-42.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular deposition of metallic fragments during phacoemulsification: possible causes and effects. Eye (Lond). 1995;9(Pt 4):434-6.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular metallic-appearing foreign bodies after phacoemulsification. J Cataract Refract Surg. 1996;22:1247-50.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular foreign bodies after cataract surgery. Arch Soc Esp Oftalmol (Engl Ed). 2018;93:598-605.
- [CrossRef] [PubMed] [Google Scholar]






