Translate this page into:
A practical guideline managing subretinal air during vitrectomy as an intraoperative complication

*Corresponding author: Daniel Cortes-Muñoz, Department of Retina and Vitreous, Instituto de Oftalmología “Fundación Conde de Valenciana”, Mexico City, Mexico. dacom10@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Illescas-Lomeli C, López-Bolaños A, Cano-Hidalgo R, Cortes-Muñoz D. A practical guideline managing subretinal air during vitrectomy as an intraoperative complication. Lat Am J Ophthalmol. 2025;8:4. doi: 10.25259/LAJO_27_2024
Abstract
A 77-year-old woman visited our office due to a 15-day decline in vision in her left eye. During the examination, she had a best-corrected visual acuity of 20/40 in her right eye and hand motion in her left eye. A binocular indirect ophthalmoscopy revealed a total rhegmatogenous retinal detachment (RRD) due to a horseshoe tear in the upper temporal quadrant. She underwent pars plana vitrectomy with a C3F8 tamponade and a scleral buckle. The procedure proceeded smoothly; however, during the fluid-air exchange, regrettably, the trocar covered the horseshoe tear, prompting the placement of subretinal air beneath the lesion. The literature worldwide has reported a limited number of cases of subretinal gas, a known but rare complication of pneumatic retinopexy to repair RRD. In this case report, we highlight the intraoperative course of this complication and describe how we managed to solve it.
Keywords
Case report
Intraoperative complication
Subretinal air
INTRODUCTION
Pars plana vitrectomy (PPV) is a relatively safe procedure widely utilized to address various vitreoretinal pathologies. In the management of rhegmatogenous retinal detachment (RRD), PPV has become increasingly common worldwide, evolving with technological advancements.[1] Despite the availability of several intraoperative options, significant variations in treatment strategies persist, such as the choice of tamponade or the use of additional scleral buckling. These differences underscore the complexity of surgical decision-making in RRD repair.
While subretinal gas is a recognized complication of pneumatic retinopexy, only a limited number of cases have reported subretinal gas after PPV.[2] Furthermore, there are no detailed descriptions of subretinal air as an intraoperative complication during PPV. This report presents the first documented case of subretinal air during PPV, offering a step-by-step guideline for its management. This complication, though possibly underreported, poses significant challenges, particularly for inexperienced surgeons, due to the lack of apposition between the neurosensory retina and the retinal pigment epithelium. Addressing this complication promptly is crucial to ensure favorable surgical outcomes.
CASE REPORT
A 77-year-old woman presented with a 15-day history of progressive vision loss in her left eye. Her medical history included cataract surgery in both eyes 15 years prior. Examination revealed a best corrected visual acuity (BCVA) of 20/40 in the right eye and hand movement in the left. Intraocular pressure (IOP), measured using Goldmann tonometry, was 20 mmHg in the right eye (OD) and 4 in the left eye (OS). Binocular indirect ophthalmoscopy showed a total RRD with a horseshoe tear in the upper temporal quadrant of the left eye.
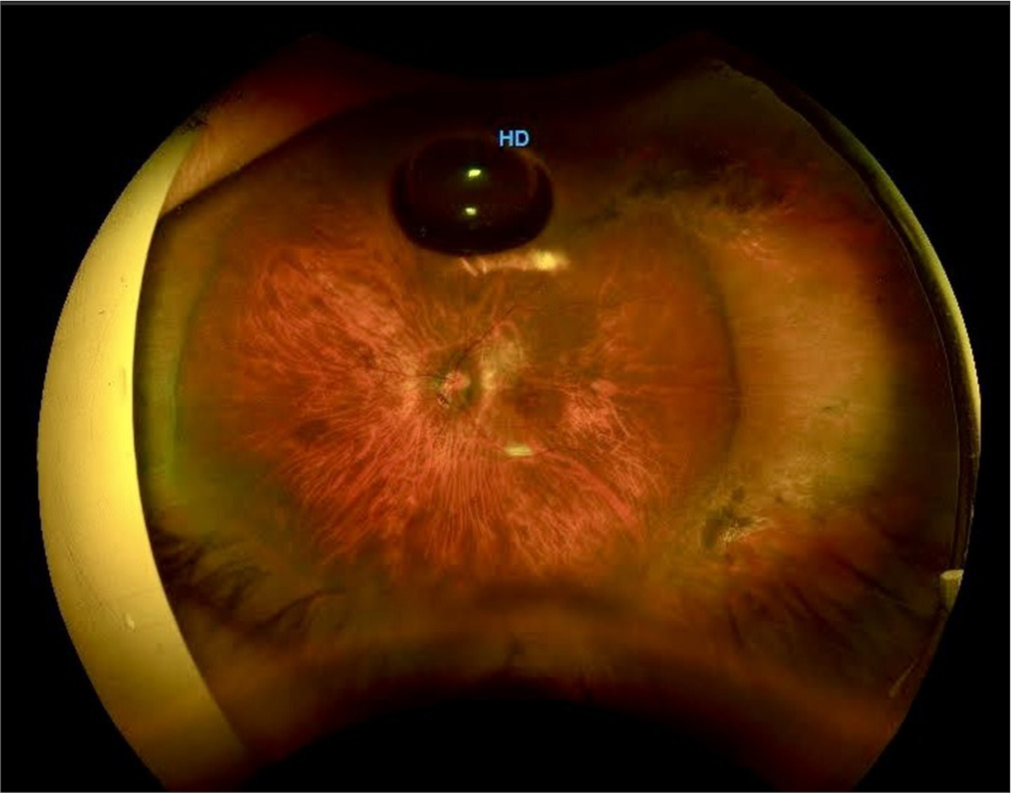
The patient underwent PPV with a C3F8 tamponade and scleral buckle placement. A 240-band was used for the scleral buckle followed by core vitrectomy using a 25-gauge system. After inducing a posterior vitreous detachment and performing peripheral vitrectomy, heavy liquids were introduced to stabilize the retina. A meticulous shave of the vitreous around the horseshoe tear released residual traction and endodiathermy was applied to mark the posterior edge of the lesion. During the fluid-air exchange (FAX), the infusion trocar inadvertently covered the horseshoe tear, resulting in the placement of subretinal air beneath the lesion [Figure 1].
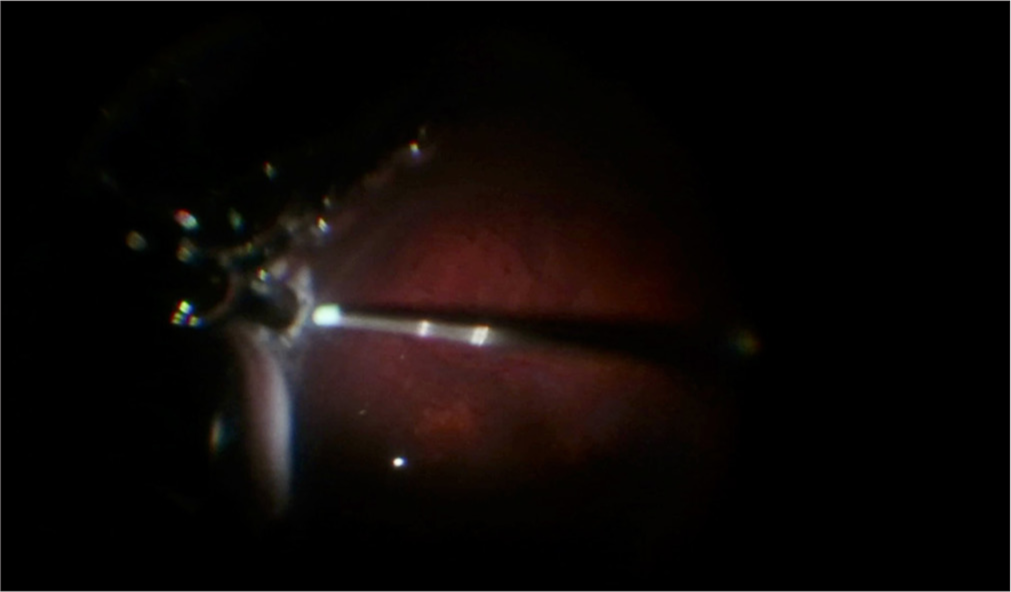
- Subretinal air during fluid-air exchange.
Management of subretinal air
The following steps were implemented to address this complication:
Perform a precise shave of the lesion: A meticulous shave of the lesion is essential to release all traction, as residual traction can lead to the accumulation of subretinal air in some cases
Ensure correct trocar position: The infusion trocar was repositioned to avoid proximity to the retinal tear, preventing further subretinal air accumulation.
-
We call this third step “The displacement:” It involves using a soft-tip cannula and a vacuum set to 350 ccs to move the subretinal air bubble through the horseshoe tear. Extreme care was taken to avoid damaging the retina [Figure 2].
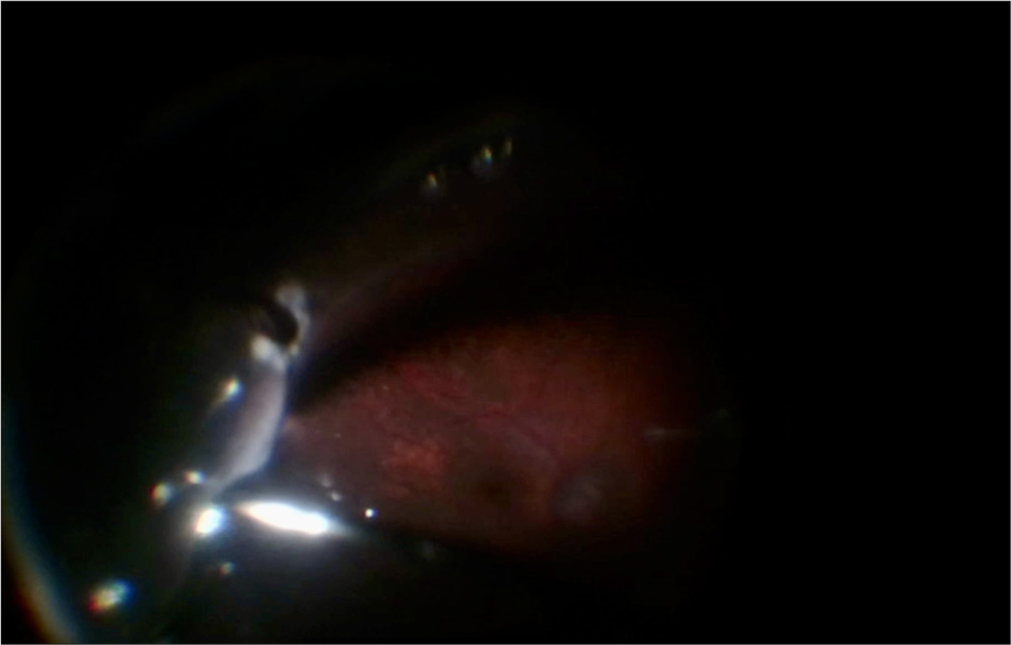 Figure 2:
Figure 2:- A soft tip maneuver within bubbles.
-
Second air-fluid exchange: If the previous maneuver is unsuccessful, the surgeon may perform a second air-fluid exchange, leveraging the tensional forces within the cavity. In our case, the exchange was carried out at an IOP of 30 mmHg for a slower FAX, although this procedure is typically performed at 45 mmHg [Figure 3].
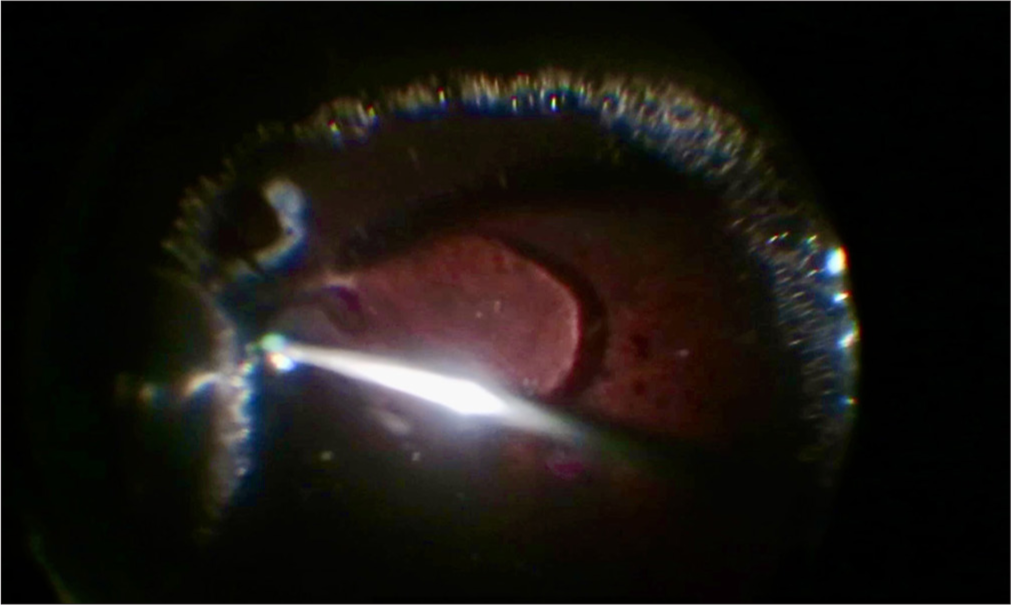 Figure 3:
Figure 3:- Air-fluid exchange.
Displacement under fluid: Subretinal air was further displaced under fluid using a soft-tip cannula. Aspiration through the retinal tear effectively removes the bubble in most cases [Figure 4].
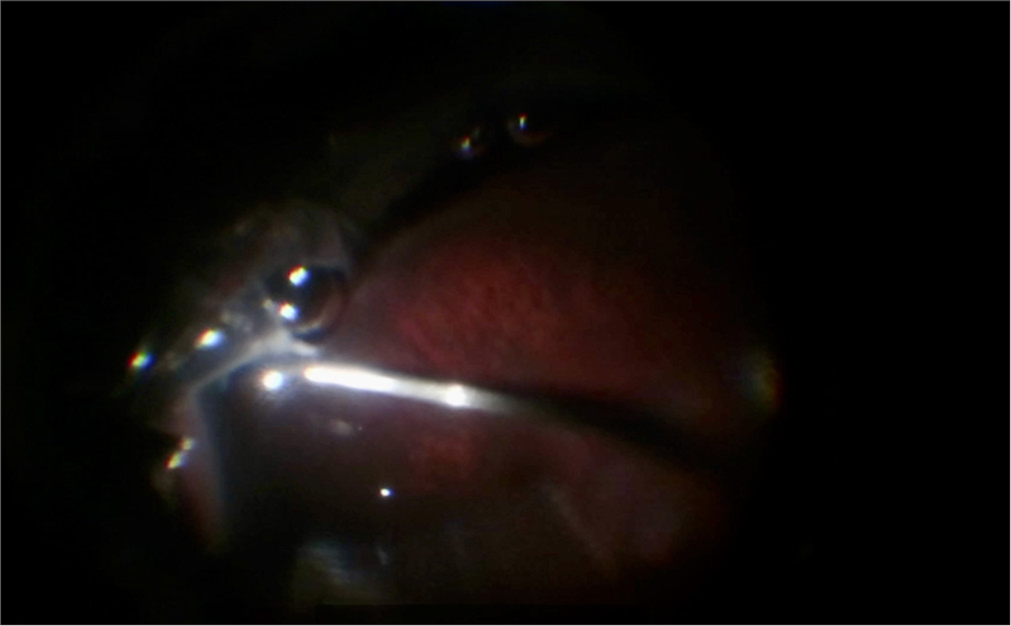
- The subretinal bubble maneuver in fluid.
In cases where these steps fail, a drainage retinotomy is recommended to release subretinal air. However, in this patient, the prior maneuvers were successful. Following bubble removal, a final FAX was performed, and photocoagulation was applied to the retinal tear. C3F8 gas was introduced as the endotamponade. Postoperatively, the subretinal bubble completely resolved, and the patient’s BCVA improved to 20/200 at 1 month and 20/60 at 2 months [Figure 5].
- Final best-corrected visual acuity of 20/60 at 2 months postoperatively.
DISCUSSION
The air-fluid exchange is a critical step in RRD surgery, as it facilitates retinal reattachment. However, it is also a stage where complications, such as subretinal air, can occur. Despite its rarity, subretinal air during PPV presents a significant challenge, particularly for less experienced surgeons.[3] Previous literature has reported subretinal gas migration after pneumatic retinopexy in approximately 3% of cases and in a few cases of PPV with air tamponade.[4] Ishiyama et al. (2022) described three cases of subretinal air appearing days postoperatively after PPV, managed with additional interventions.[5] However, there remains a lack of standardized guidelines for intraoperative management of subretinal air.
This case highlights the importance of prompt recognition and meticulous intraoperative management to prevent adverse outcomes. Key lessons include ensuring proper trocar placement, effectively utilizing FAXs, and employing a soft-tip cannula for bubble displacement. Future studies could explore whether subretinal air is more common than currently reported, emphasizing the need for standardized guidelines.
In addition, a recent report by Seamone et al. (2019) described a similar complication of subretinal gas following PPV for RRD. The authors outlined a successful management strategy involving external drainage, FAX, and posterior retinotomy. These steps enabled the effective removal of subretinal gas and facilitated retinal reattachment, underscoring the importance of a systematic approach to address such complications. This report reinforces the need for vigilance during gas-air exchanges to optimize surgical outcomes.[6]
CONCLUSION
The successful management of intraoperative complications, such as subretinal air during PPV, is crucial for optimal visual outcomes. This case underscores the importance of careful surgical technique, prompt recognition of complications, and a systematic approach to management. While subretinal air is a rare complication, the steps outlined in this report provide a practical guide for vitreoretinal surgeons, particularly those with limited experience.
Further research is warranted to determine the prevalence of this complication and develop comprehensive guidelines for its management. Establishing such protocols could enhance surgical outcomes and minimize the risk of complications in vitreoretinal surgery.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
René Cano-Hidalgo is on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- The pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial (PIVOT) Ophthalmology. 2019;126:531-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pneumatic retinopexy: A critical reappraisal. Surv Ophthalmol. 2021;66:585-93.
- [CrossRef] [Google Scholar]
- Pneumatic retinopexy: An experience of 12 years at a tertiary care hospital. Cureus. 2023;15:e46180.
- [CrossRef] [PubMed] [Google Scholar]
- The management of subretinal gas following attempted pneumatic retinal reattachment. Ophthalmology. 1987;94:319-26.
- [CrossRef] [PubMed] [Google Scholar]
- Subretinal air migration after pars plana vitrectomy and air tamponade for rhegmatogenous retinal detachment. Am J Ophthalmol Case Rep. 2022;25:101279.
- [CrossRef] [PubMed] [Google Scholar]
- Massive subretinal gas after vitrectomy surgery: Mechanism and management. Retin Cases Brief Rep. 2019;13:266-8.
- [CrossRef] [PubMed] [Google Scholar]







