Translate this page into:
Atypical orbital cellulitis in a leprosy patient –A diagnostic and therapeutic challenge

*Corresponding author: Bijnya Birajita Panda, Department of Ophthalmology, All India Institute of Medical Sciences, Bhubaneswar, Odisha, India. bigyan_panda@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Panda BB, Agarwal U, Sable M, Ayyanar P. Atypical orbital cellulitis in a leprosy patient – A diagnostic and therapeutic challenge. Lat Am J Ophthalmol. 2025;8:6. doi: 10.25259/LAJO_37_2024.
Abstract
Leprosy is primarily a disease of the skin and peripheral nerves; its association with malignancies in atypical sites like the orbit is exceedingly rare. The diagnostic challenge arises from overlapping clinical features of leprosy-induced inflammation and malignancy, often leading to delays in diagnosis and treatment. We present the case of a male in his fifties with a history of treated leprosy who presented with progressive proptosis, orbital swelling, and a frozen globe. Initial evaluation suggested orbital cellulitis or granulomatous inflammation secondary to residual leprosy. Imaging revealed poorly demarcated orbital mass involving the extraocular muscles and optic nerve, raising suspicion for malignancy. Histopathological examination of the orbital biopsy confirmed a diagnosis of T-cell lymphoma.
Keywords
Immunohistocytochemistry
Leprosy
Orbital cellulitis
T-cell lymphoma
INTRODUCTION
Orbital cellulitis is a severe infectious condition that typically arises due to bacterial or fungal pathogens. However, in rare instances, atypical presentations may mask underlying malignancies. Here, we present a unique case of a patient with a history of leprosy who initially presented with signs of orbital cellulitis but was ultimately diagnosed with extranodal natural killer/T (NK/T) cell lymphoma upon biopsy. This case highlights the importance of considering malignant etiologies in patients with atypical or refractory orbital infections.
DISCUSSION
Orbital malignancies often represent a diagnostic dilemma for clinicians, given their varying and atypical presentations. We report the case of a 52-year-old male, a known case of tuberculoid leprosy on multi-drug therapy (Dapsone, rifampicin, and clofazimine) for 8-month duration, presented with gradual diminution of vision in the right eye with sudden worsening of symptoms for 1-week. On examination, there was no perception of light in the right eye and 6/18 in the left eye. Dilated fundus evaluation in the right eye revealed hazy media due to exposure keratopathy. His left eye was within normal limits. During the course of 2 days, he developed painful, tense swelling in eyelids, complete restriction of eye movements, and a dilated fixed pupil in the right eye [Figure 1a]. To note, there was development raised, erythematous plaque such as skin lesions in the ear lobule, trunk, and thighs associated with spikes of fever and significant weight loss during his stay in the hospital [Figure 1b and c]. A computed tomography scan was suggestive of the right-sided orbital cellulitis with optic nerve stretch [Figure 1d]. He was administered with broad-spectrum antibiotics and anti-inflammatory agents but the condition did not improve. In view of a painful blind eye, an enucleation was performed, and the suspicious orbital tissue and eyeball were sent for histopathology. He developed right foot drop and sensory loss over the nerve supply areas of the right side tibial and femoral nerves. A multi-specialty consultation with a neurologist and dermatologist suggested that the patient had borderline tuberculoid leprosy, which was downgrading to lepromatous leprosy, with a possible lepra reaction. The patient was started on continued on multi drug treatment (MDT) and oral prednisone, and an incisional biopsy of the skin lesion from the thigh was sent for histopathological examination. Histopathology of the skin lesion revealed a diagnosis of natural killer/T (NK-T)-cell lymphoma [Figure 1e]. To our surprise, similar histopathological findings were seen in the sclera and orbital tissue, which were supported by immunohistochemistry staining at both places [Figure 1f]. A final diagnosis of NK/T-cell lymphoma was made, and the patient was referred to a medical oncologist, where they started him on four cycles of L-asparagine 6000 U/m2, methotrexate 3 mg/m2, and dexamethasone 40 mg. The skin lesions started to resolve early within a week. The guarded prognosis was explained to the patient. He was given an artificial prosthesis for the right eye and is in regular follow-ups for the past 2 years without any recurrence. In India, where leprosy is endemic, its reactional episodes can mimic other conditions, making the diagnosis challenging.[1] Few authors have reported about the association of leprosy and visceral, lymphoreticular malignancies, malignant T-cell lymphoma, and peripheral T-cell lymphoma; however, in all these reports, ocular involvement was not seen.[2-4] Furthermore, there are few reported cases of NK/T-cell lymphoma presenting as orbital cellulitis in association with nasal sinus involvement.[5,6] However, orbital T-cell lymphoma with scleral invasion presenting as cellulitis in the absence of sinusitis or any form of nasal involvement leading to the diagnosis of systemic T-cell lymphoma in a leprosy patient is the first of its kind to be reported to date.
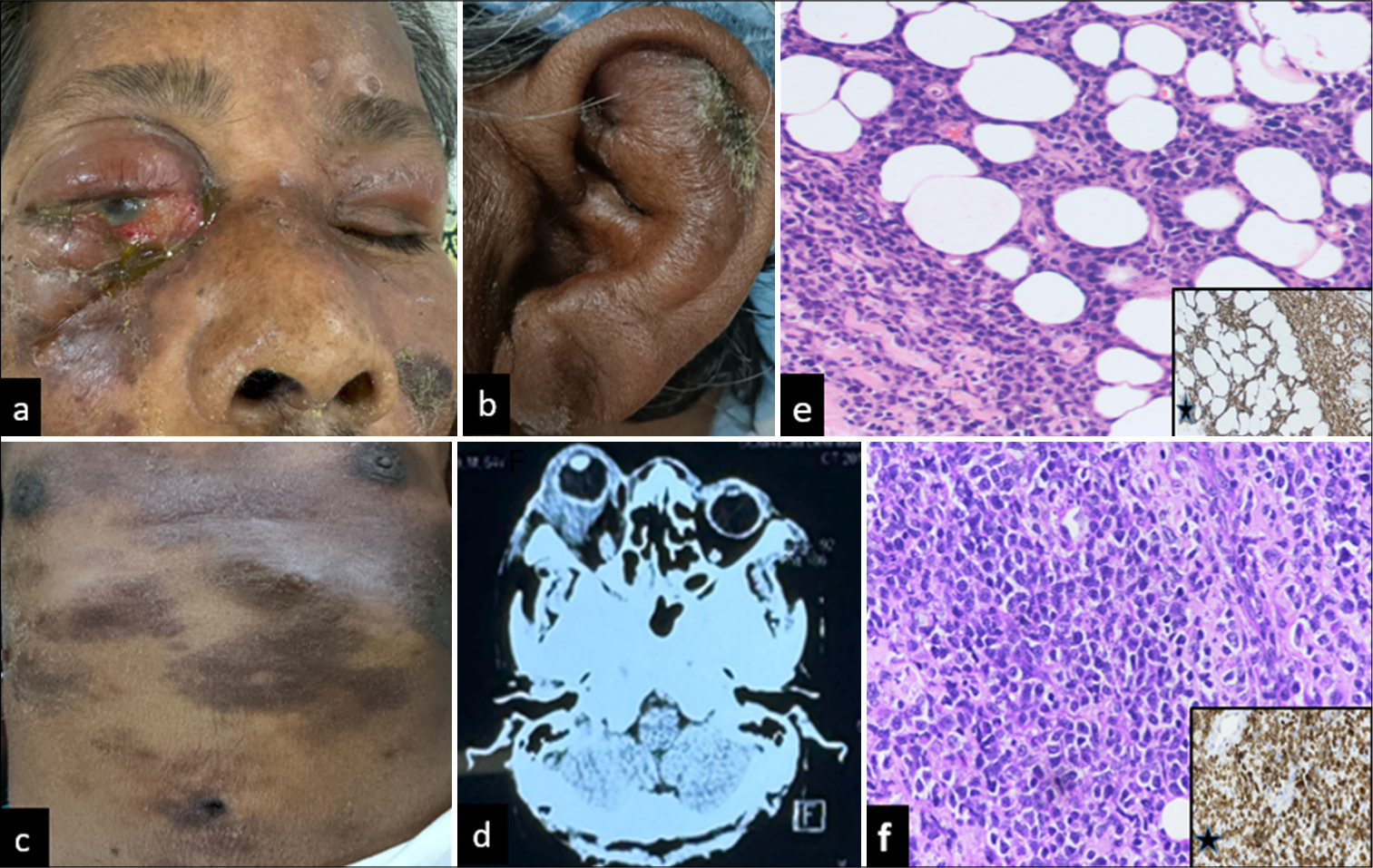
- (a) Clinical photo showing a frozen globe due to tense orbital cellulitis and indurated skin in the periorbital area. (b and c) Multiple erythematous raised, plaque-like lesions over the ear lobule, trunk, and abdomen suggestive of systemic spread of disease. (d) Axial computed tomography scan is suggestive of diffuse soft-tissue mass surrounding the globe in the intraconal and extraconal spaces. (e) Histopathology of skin lesion biopsy hematoxylin and eosin (H&E) stain ×20 showing atypical lymphoid cells with irregular nuclear membrane, immunohistocytochemistry (IHC) staining showing cluster differentiation (CD) 3 positive cells suggestive of cutaneous T-cell lymphoma (star marking in inset view) (f) Histopathology of the suspicious area of sclera H&E stain ×20 showing atypical lymphoid cells with a round nucleus and prominent nucleoli, IHC staining showing CD 3 positive cells suggestive of extranodal natural killer/T (NK/T)-cell lymphoma (star marking in inset view).
A careful general examination of any skin lesion and lymph node examination should be performed while managing orbital cellulitis in patients with co-existing systemic disease. Scleral tissue excised after evisceration should be sent for histopathological examination since they can also be an important marker of an underlying systemic condition causing panophthalmitis.
CONCLUSION
This case underscores the necessity of maintaining a high index of suspicion for masquerading malignancies in patients with atypical orbital cellulitis, particularly in those with predisposing immunological or infectious conditions. Early biopsy and histopathological evaluation played a crucial role in achieving the correct diagnosis, allowing timely initiation of chemotherapy. The patient responded well to treatment, emphasizing the importance of early recognition and targeted therapy in improving clinical outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Epidemiological scenario of leprosy in marginalized communities of India: Focus on scheduled tribes. Indian J Med Res. 2022;156:218-27.
- [CrossRef] [PubMed] [Google Scholar]
- Leprosy in a patient with lymphoma: A challenge in the twenty-first century. Cureus. 2023;15:e50007.
- [CrossRef] [Google Scholar]
- Malignant T-cell lymphoma mimicking lepromatous leprosy. Clin Exp Dermatol. 2001;26:173-5.
- [CrossRef] [PubMed] [Google Scholar]
- Leprosy and malignancy: Autopsy findings of 252 leprosy patients. Int J Lepr. 1990;58:697-702.
- [Google Scholar]
- Extranodal natural killer/T-cell lymphoma presenting as orbital cellulitis. GMS Ophthalmol Cases. 2017;7:Doc04.
- [Google Scholar]
- Orbital lymphoma masquerading as orbital cellulitis. Case Rep Ophthalmol Med. 2021;2021:8832783.
- [CrossRef] [PubMed] [Google Scholar]







