Translate this page into:
Bilateral dense persistent pupillary membrane - A rare case

-
Received: ,
Accepted: ,
How to cite this article: Chaurasiya SK, Vanrammuana, Tep H, Singh M. Bilateral dense persistent pupillary membrane - A rare case. Lat Am J Ophthalmol 2023:6:13.
Abstract
A persistent pupillary membrane (PPM) is a congenital eye condition characterized by the presence of remnants of tissue in the eye that normally regresses during fetal development. A 37-year-old male patient complained of bilateral blurred vision for distance that had been present from childhood and was accompanied by glare and photophobia. On examination, uncorrected distance visual acuity was 20/30 in the right eye and 20/40 in the left eye, and there was no improvement with pinhole. The slit-lamp examination showed PPM with covering pupil partially in both eyes. The management of PPM depends on the severity of the condition and its impact on vision and ocular health.
Keywords
Persistent pupillary membrane
Dense
Amblyopia
INTRODUCTION
Persistent pupillary membrane (PPM) is a common congenital ocular abnormality that affects 20% of adults and 95% of newborns. It appears as tiny strands of iris along the pupil and is made up of the anterior tunica vasculosa lentis, which in the first 6 months of fetal life feeds the crystalline lens.[1,2] It can very rarely show as a whole dense membrane, and we provide a case-based approach to this membrane in a 37-year-old male patient.
CASE
A 37-year-old northern male patient presented to the hospital with complaints of blurring of vision, photophobia, and glare in both eyes since childhood. There is no history of wearing spectacle in the past. Other history was not significant.
On examination, his right eye (RE) and left eye (LE) unaided distance visual acuity (VA) was found to be 20/30 and 20/40, respectively, which did not improve with pinhole, whereas for near, the VA was N12 in both eyes. A very dull glow was obtained on dry retinoscopy as there was media opacity. Post-dilatation with tropicamide 0.8% and phenylephrin 5%, wet retinoscopy revealed objective refraction of RE +5.00/−5.00 × 80 and LE +7.00/−5.50 × 80; however, the patient did not accept any correction in both eyes and VA also remained unchanged.
On slit-lamp examination, clear corneas, quiet and deep anterior chambers, with dense membrane occluding the pupillary area which was continuous with the collarette were observed in both eyes [Figure 1a and b]. Baseline intraocular pressure measured with Goldmann applanation tonometry was 20 and 23 mmHg for RE and LE, respectively, which was corrected to 18 and 21 mmHg according to the linear formula; corrected intraocular pressure (IOP) = measured IOP-(Central corneal thickness- 545)/50 × 2.5 mmHg.[3] Anterior chamber angle was open up to scleral spur in both eyes as observed on gonioscopy (Zeiss 4 mirror). Bilaterally, crystalline lenses were clear, and fundus was normal with cup disc ratio of 0.2. A-scan biometry using LENSTAR LS 900 (Haag Streit, USA) revealed axial length of the eyeballs to be 22.68 mm and 22.14 mm in RE and LE, respectively. Keratometry values (K1 and K2) for RE 42.13 D × 67° and 45.39 D × 157° and for LE 42.13 × 90, 45.87 × 180, respectively. Systemic examination revealed no association. A clinical diagnosis of PPM was made based on ocular findings. Due to the late presentation with uncorrected refractive error, the patient also developed ametropic amblyopia and VA was quiet manageable, any surgical intervention was deferred.
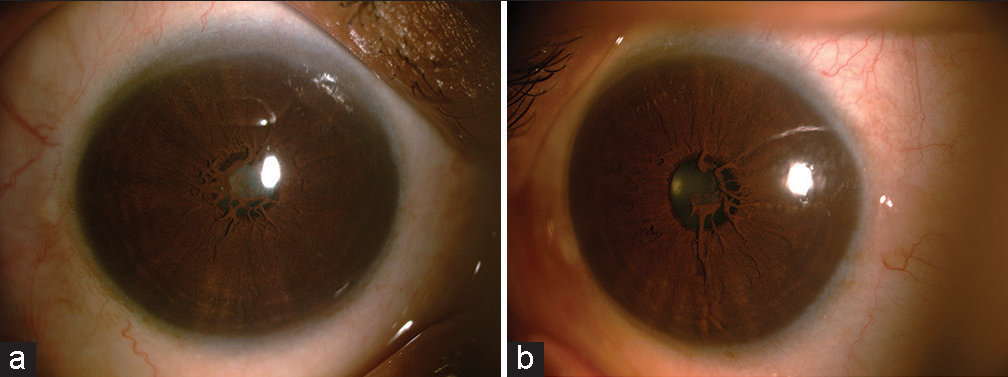
- (a and b) Dense membrane occluding the pupillary area which is continuous with the collarette.
DISCUSSION
By 9 weeks of gestation, the pupillary membrane, the remaining anterior section of the tunica vasculosa lentis, is often fully grown, and by 34 weeks, it has usually disappeared.[4] When a baby is delivered, especially if they are premature, it is not unusual to see some of the pupillary membrane. In most cases, these remnants are asymptomatic, and they eventually atrophy. Only mydriatic agents and occlusion therapy can be administered to them since they do not need any medical attention or treatment.[5] However, in other instances, multiple continuous membranes obstructing the pupillary axis may occur with or without other visual problems and may need surgical treatment. Multiple authors have reported PPM associated with other anterior chamber anomalies but a few cases have been reported on only PPM so far. PPMs may be inherited autosomal dominant along with other anterior chamber defects such goniodysgenesis and aniridia.[5-7] In our cases, no family history had PPMs. PPM can sometimes be associated with amblyopia, if it obstructs the visual axis, causes significant visual blur, or induces refractive errors (e.g., astigmatism) that are not properly corrected. In such cases, the brain may suppress the visual input from the eye affected by the PPM, leading to poor visual development and amblyopia.
CONCLUSION
Timely detection and appropriate management of PPM-related visual issues are crucial to prevent or treat amblyopia. If the PPM is causing visual impairment, intervention through surgical removal, laser treatment, or optical corrections can help improve VA and reduce the risk of amblyopia.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A rare case of persistent pupillary membrane: Case-based approach and management. Indian J Ophthalmol. 2018;66:1480-3.
- [CrossRef] [PubMed] [Google Scholar]
- Duane’s ophthalmology Philadelphia, PA: Lippincott Williams and Wilkins; 2007. p. :24-258. Available from: http://ovidsp.ovid.com/ovidweb.cgi?t=js&page=booktext&news=n&df=bookdb&an=01222986/2007_edition/11&xpath=/pg(0) [Last accessed on 2023 Sep 28]
- [Google Scholar]
- Clinical significance of central corneal thickness in the management of glaucoma. Arch Ophthalmol. 2004;122:1270-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperplastic persistent pupillary membrane-surgical management. J Pediatr Ophthalmol Strabismus. 1983;20:149-52.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperplastic persistent pupillary membranes with congenital corneal anomalies. J Cataract Refract Surg. 2007;33:1123-6.
- [CrossRef] [PubMed] [Google Scholar]
- Ectopia lentis et pupillae syndrome in three generations. Br J Ophthalmol. 1995;79:135-8.
- [CrossRef] [PubMed] [Google Scholar]
- Persistent pupillary membrane associated with aniridia. Am J Ophthalmol. 1978;86:118-20.
- [CrossRef] [PubMed] [Google Scholar]






