Translate this page into:
Modified packing technique in large traumatic macular holes

*Corresponding author: Jesus Hernan Gonzalez-Cortes, Department of Ophthalmology, Autonomous University of Nuevo Leon, University Hospital and Faculty of Medicine, Monterrey, Nuevo Leon, Mexico. drjesusgzz@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Gonzalez-Cortes JH, Treviño-Herrera AB, Padilla-Alanis ST, Gonzalez-Cantu JE, Lozano-Rodriguez JR, Pelayes D. Modified packing technique in large traumatic macular holes. Lat Am J Ophthalmol. 2024;7:13. doi: 10.25259/LAJO_9_2024
Abstract
Autologous internal limiting membrane (ILM) flap techniques have been demonstrated to increase the incidence of successful closure in large traumatic macular holes (TMHs). Different ILM flap manipulation and placement approaches have been described, including the non-inverted free ILM flap and the inverted ILM flap techniques. The usage of viscoelastic fluids and perfluorocarbon heavy liquids has been described to achieve proper ILM flap positioning in idiopathic macular holes(MH). We describe a modified ILM packing technique for the treatment of large TMH entitled “fill in the hole” and we present the anatomical and visual results in two cases. We also present a step-by-step video describing the “fill in the hole” technique.
Keywords
Internal limiting membrane flap
Internal limiting membrane peeling
Macular hole
Traumatic macular hole
INTRODUCTION
Full-thickness macular hole (FTMH) is defined as a full-thickness defect of the neuroretina in the foveal area. A traumatic macular hole (TMH) is the result of direct or indirect trauma to the eyeball. TMH accounts for 5–8.2% of the etiology of all FTMH.[1] The prevalence of TMH is higher in men than in women (86.3% vs. 27.7%) and young males tend to be more affected.[2] The incidence of TMH following an open-globe injury is 0.15%, and in blunt trauma is 1.4%.[3,4] Due to the low incidence of TMH, a preferred therapeutic approach or guideline for this condition has not been established and there are multiple options for its management. The treatment modalities include observation and surgery.
Multiple surgical techniques have been described and include pars plana vitrectomy (PPV) with or without internal limiting membrane (ILM) peeling and silicone oil or gas as tamponades. Different adjuvant therapies have been reported, such as transforming growth factor beta (TGF-β), biological tissue adhesives, autologous serum, and platelet concentrate.[3] Different ILM grafting techniques have been described in the treatment of FTMH.[5-7] Furthermore, an autologous retinal graft technique has been used for large TMH with good anatomical results but limited visual results.[8]
The objectives of this report are to describe a modified ILM packing technique in large TMH, to describe the optical coherent tomography (OCT) closure features, and to report the final visual outcome. This surgical technique was presented at the EuroLam Congress (Quito, Ecuador) in 2018 and at the Euretina Congress (Paris, France) in 2019.
Surgical technique
Phacoemulsification with intraocular lens implantation was performed if a cataract was present.
A standard 3-port 25 G PPV was performed under retrobulbar anesthesia. Core vitrectomy was completed, followed by triamcinolone acetonide (TA)-assisted posterior hyaloid removal (40 mg/mL) and peripheral vitrectomy.
ILM staining was achieved with brilliant blue G 0.025% stain. In addition, we injected a small amount of TA. Excess stains and TA were removed, and a 0.5 cc bubble of perfluorocarbon liquid (PFCL) was injected within the temporal vascular arcades. Through the PFCL bubble, direct forceps grasping of the ILM was delicately performed and an ILM parafoveal flap was created at 1.5 discs diameters temporal to the macular hole (MH). ILM peeling was completed in a circular fashion way, taking care not to peel the flap from the MH margin and carefully placing all the free ends inside of the MH [Video 1]. Subsequently, a peripheral extension of the ILM peeling was performed, followed by fluid-air exchange and PFCL removal [Figures 1 and 2]. Gas exchange with 20% SF6 was done to conclude the procedure. Face down position/prone position was indicated for 5 days.
Video 1:
Video 1:Step-by-step video of the modified packing technique in large traumatic macular holes.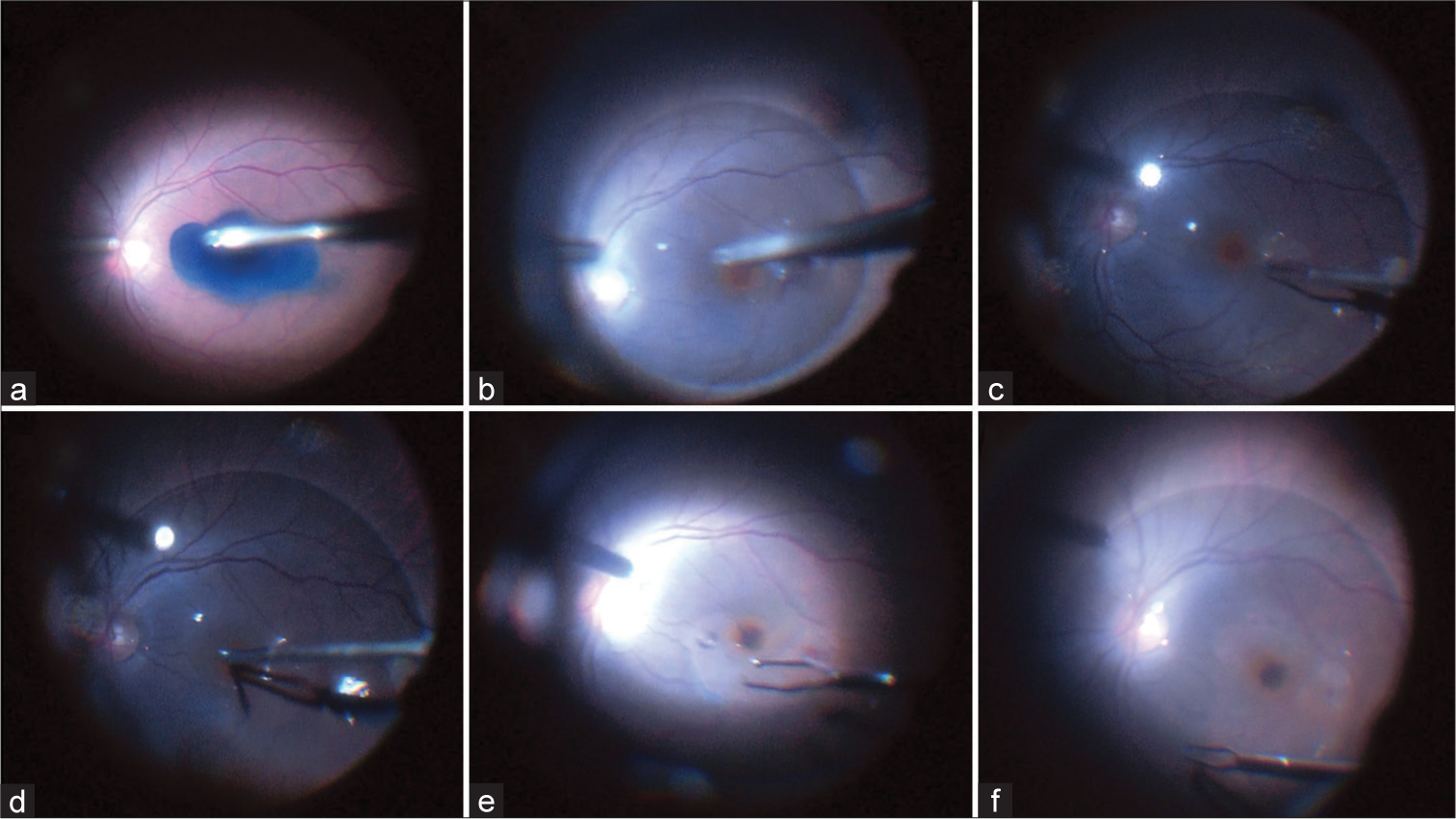
- Step-by-step modified packing technique in large traumatic macular holes. (a) Internal limiting membrane (ILM) staining with brilliant blue G 0.025%. (b) perfluorocarbon liquid is applied in the macular area. (c) ILM peeling. (d and e) Packing the macular hole with the ILM. (f) Peripheral extension of the ILM peeling.
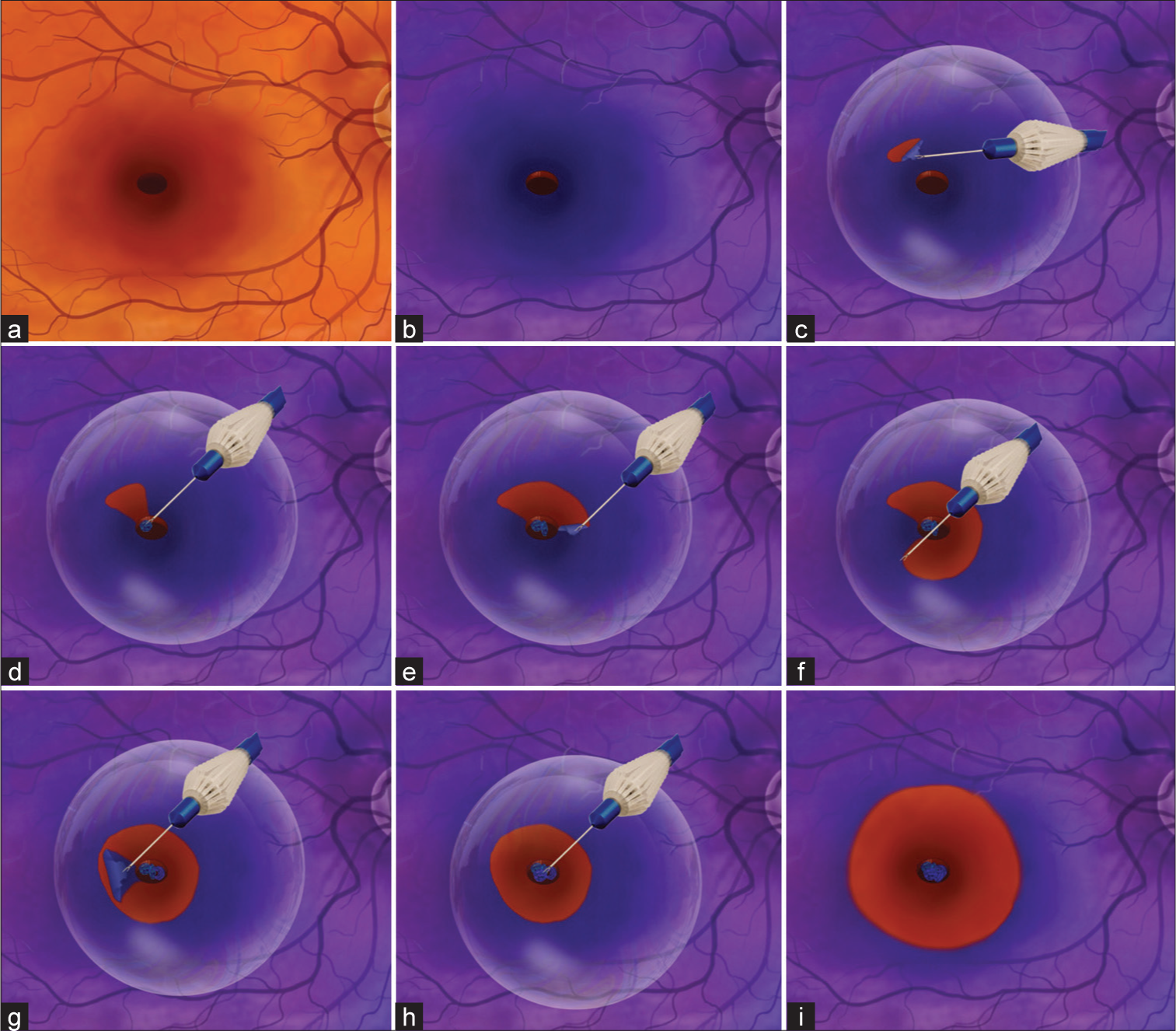
- Modified packing technique in large traumatic macular holes scheme. (a) Macular hole (MH). (b) Internal limiting membrane (ILM) staining with brilliant blue G 0.025%. (c-f) ILM peeling under perfluorocarbon liquid. (g and h) Packing the MH with the ILM. (i) Peripheral extension of the ILM peeling.
CASE SERIES
Case 1
A 43-year-old male patient with a history of left eye (LE) blunt ocular trauma with fist presented to the emergency department. The patient complained of a central visual field defect. His LE best-corrected visual acuity (BCVA) was 20/800. The examination showed a large traumatic full-thickness MH and a superior peripapillary choroidal rupture. Spectral-domain OCT (SD-OCT) revealed a giant (1200 microns) full-thickness defect of retinal layers, intraretinal cyst-like spaces at the margins, a subretinal hyporeflective area suggestive of subretinal fluid, and absence of posterior vitreous detachment (PVD). Four weeks postoperative, SD-OCT showed the ILM graft within the closed MH. Twelve weeks after surgery, the BCVA was 20/200 with a closed MH. SD-OCT showed type 1 MH closure with improvement in the organization of the ellipsoid layer.
Case 2
A 61-year-old female with a 3-month history of a TMH came for a second opinion. She was diagnosed elsewhere and advised for observation, waiting for spontaneous closure. The patient complained of central scotoma since the presentation. Her BCVA was 20/400 and the SD-OCT image revealed a giant full-thickness TMH (814 microns) with thickened and raised edges. There was the presence of intraretinal cyst-like spaces in the outer and inner nuclear layers and complete foveal posterior hyaloid detachment. Four weeks after surgery, SD-OCT showed the ILM graft within the MH. Twelve weeks after surgery, the BCVA was 20/80 with a closed MH. The SD-OCT image showed type 1 MH closure with improvement in the organization of the ellipsoid layer.
DISCUSSION
The exact mechanism for the formation of a TMH is not fully understood, and several theories have been formulated. The most widely accepted theory establishes that after blunt trauma, an anteroposterior compression with an equatorial expansion of the globe causes sudden vitreomacular traction and avulsion of the retinal tissue. During rebound, the tangential traction force between the vitreous and retina forms the TMH.[1] The rate of spontaneous closure of TMHs ranges from 10.7% to 44.4%.[9-11] Several investigators suggest waiting up to 3 months for spontaneous closure of the TMH to avoid severe damage to the photoreceptors.[9] Spontaneous closure of the TMH may still occur after 3 months, although it is less likely to occur.
Multiple surgical techniques have been developed over time with the sole purpose of closing the TMH. Wendel et al. first described the vitreoretinal surgery for idiopathic MHs, which consisted of PPV, PVD induction, epiretinal membrane peeling, fluid-gas exchange, and 1 week of face-down position. With this intervention, they reported an 80% anatomic success rate.[12] Rubin et al. described that surgery combined with TGF-β 2 achieved a 67% single-surgery closure rate of TMH.[13] Platelet concentrates in combination with surgery can help improve anatomical and functional results, with an 86% single-surgery success rate and 100% of eyes with at least two lines of visual improvement.[14,15] Autologous human serum in conjunction with vitrectomy in TMH eyes has reported a 100% success rate with two or more lines of visual improvement in 75% of the eyes.[16] Kuhn et al. described the ILM peeling technique using SF6 as tamponade for TMH. They reported a single-surgery closure rate of 100% with most of the patients with at least two lines of improvement.[4] Similarly, Bor’i et al. reported a 92% single-surgery closure rate.[17]
Michalewska et al. described the ILM inverted flap technique for idiopathic FTMH, which consists of a circumferential peeling of the ILM without removing it completely, remaining partially attached to the edges of the MH. A coiled segment of the peeled ILM remains dangling in the vitreous cavity. The peripheral pieces of the ILM are trimmed, leaving the central part. The ILM is then placed over the MH until it is inverted and the surface that normally faces the vitreous now faces downwards towards the RPE.[6] The hypothesis for MH closure using this technique is that filling off the hole with proliferating cells enhances closure. It is also suggested that it may act as a scaffold for cell proliferation. Also, the peeled ILM contains fragments of Müller cells that can induce gliosis. Abou Shousha described the usage of the ILM inverted flap technique with SF6 tamponade for TMH. They reported a closure rate of 100% with a median final visual acuity of 20/100.[18] A variety of this technique is the ILM autologous transplantation technique described by Morizane et al. This technique consists of the colocation of autologous ILM-free flap in the MH covered with viscoelastic material.[19]
Singh and Narayanan described the autologous retinal graft technique for a large TMH. It consists of obtaining a retinal graft; endo laser is applied around the donor site, followed by endocoagulation of the bleeder vessels and the retinal graft dissection. The graft is then tucked or flattened over the MH, facilitated with PFCL, and silicon oil is used as tamponade.[8]
In the present article, we present the modified packing technique for large TMHs entitled “fill in the hole” technique, which consists of seven steps [Video 1, Figures 1 and 2]. 1, PPV; 2, Triamcinolone assisted posterior hyaloid removal; 3, ILM staining; 4, PFCL injection; 5, ILM peeling under PFCL (without removing from the edges of the MH); 6, Packing the MH with the ILM as an inverted flap under PFCL; 7, Fluid-gas exchange (SF6). Using the present technique, single-surgery type 1 closure was achieved in both cases presented. The final visual acuity improved from 20/800 to 20/200 and from 20/400 to 20/80 for cases 1 and 2, respectively. Moreover, in the SD-OCT analysis, 12 weeks after surgery, an improvement in the organization of the external limiting membrane (ELM) and the ellipsoid zone (EZ) was noted in both cases, which correlated with the visual acuity (VA) improvement. The present technique presents multiple advantages, it permits a controlled manipulation of the flap during the peeling [Figure 1c and d] and during the packing, prevents separation of the ILM from the edge of the TMH [Figure 1e], and reduces the risk of inadvertent suction of the ILM graft during the fluid-air exchange. Triamcinolone is used intraoperatively for marking and anti-inflammatory purposes. The vitreous and the ILM can be better assessed using triamcinolone. Gonzalez-Cortes et al. demonstrated with intraoperative optical coherence tomography, that during the removal of the ILM, both the flap and flap edges were more clearly identified when triamcinolone was used as a vitreomacular interface marker compared to brilliant blue. [20] On the other hand, Ehlers et al. also reported that triamcinolone injection revealed increased hyperreflectivity in the posterior hyaloid, which could not be achieved with brilliant blue.[21] In our technique, triamcinolone was considered to provide better identification of the ILM and to increase the precision of its manipulation during its removal through the PFCL. Multiple studies compared different tamponade agents for TMH surgery. In the present technique, SF6 was used as a tamponade along with 5 days of face-down position, this was sufficient to achieve the TMH closure.
In the present report, VA improvement of at least 2 lines was achieved in both of our patients.
CONCLUSION
The present technique of ILM inverted flap technique under PFCL for TMH may allow safe control in the manipulation and packing of the ILM into the TMH, may prevent separation of the ILM from the edge of the MH, and may reduce the risk of inadvertent suction of the ILM graft during the fluid-air exchange. However, our case report is illustrative and prospective randomized, long-term studies are needed to better determine the success rates and possible specific indications according to the characteristics of the TMH.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Jesus Hernan Gonzalez-Cortes and Dr. David Pelayes are on the Editorial Board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Videos available on:
Financial support and sponsorship
Nil.
References
- Cell composition at the vitreomacular interface in traumatic macular holes. Graefes Arch Clin Exp Ophthalmol. 2022;260:873-84.
- [CrossRef] [Google Scholar]
- Management modalities for traumatic macular hole: A systematic review and single-arm meta-analysis. Curr Eye Res. 2017;42:287-96.
- [CrossRef] [Google Scholar]
- Traumatic macular hole: Diagnosis, natural history, and management. J Ophthalmol. 2019;2019:5837832.
- [CrossRef] [Google Scholar]
- Internal limiting membrane removal for traumatic macular holes. Ophthalmic Surg Lasers. 2001;32:308-15.
- [CrossRef] [Google Scholar]
- Multi-layer internal limiting membrane plug technique for management of large full-thickness macular holes. Int J Retina Vitreous. 2022;8:80.
- [CrossRef] [Google Scholar]
- Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018-25.
- [CrossRef] [Google Scholar]
- Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229-30.
- [CrossRef] [Google Scholar]
- Functional and morphological evaluation of autologous retinal graft in large traumatic macular hole. Indian J Ophthalmol. 2019;67:1760-2.
- [CrossRef] [Google Scholar]
- Spontaneous closure of traumatic macular hole. Am J Ophthalmol. 2002;133:230-5.
- [CrossRef] [Google Scholar]
- Prediction of spontaneous closure of traumatic macular hole with spectral domain optical coherence tomography. Sci Rep. 2015;5:12343.
- [CrossRef] [Google Scholar]
- Vitrectomy, fluid-gas exchange and transforming growth factor--beta-2 for the treatment of traumatic macular holes. Ophthalmology. 1995;102:1840-5.
- [CrossRef] [Google Scholar]
- Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol. 1995;233:549-54.
- [CrossRef] [Google Scholar]
- The role of vitreoretinal surgery in the treatment of posttraumatic macular hole. Retina. 1997;17:372-7.
- [CrossRef] [Google Scholar]
- Traumatic macular hole: Observations, pathogenesis, and results of vitrectomy surgery. Ophthalmology. 2001;108:853-7.
- [CrossRef] [Google Scholar]
- Pars plana vitrectomy with internal limiting membrane peeling in traumatic macular hole: 14% perfluoropropane (C(3)F(8)) versus silicone oil tamponade. J Ophthalmol. 2017;2017:3917696.
- [CrossRef] [Google Scholar]
- Inverted internal limiting membrane flap for large traumatic macular holes. Medicine (Baltimore). 2016;95:e2523.
- [CrossRef] [Google Scholar]
- Autologous transplantation of the internal limiting membrane for refractory macular holes. Am J Ophthalmol. 2014;157:861-9.e1.
- [CrossRef] [Google Scholar]
- Anatomical changes of full-thickness macular hole documented by microscope-integrated spectral-domain optical coherence tomography. Ophthalmic Surg Lasers Imaging Retina. 2018;49:e105-11.
- [CrossRef] [Google Scholar]
- Contrast-enhanced intraoperative optical coherence tomography. Br J Ophthalmol. 2013;97:1384-6.
- [CrossRef] [Google Scholar]






