Translate this page into:
Ocular filariasis in the form of a conjunctival granuloma – A rare case report from non-endemic part of India

*Corresponding author: Annesha Sarkar, Department of Ophthalmology, Sri Sankardeva Nethralaya, Guwahati, Assam, India. annesha.anni10@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sarkar A, Das D, Islam S, Deka A. Ocular filariasis in the form of a conjunctival granuloma – A rare case report from non-endemic part of India. Lat Am J Ophthalmol. 2024;7:7. doi: 10.25259/LAJO_1_2024
Abstract
Filariasis, a predominantly lymphatic disease can rarely have ocular involvement in endemic as well as a few non-endemic zones of the Indian subcontinent. It has also been reported from countries of South East Asia. In India, Wuchereria bancrofti and Brugia malayi are the nematodes causing filariais. Ocular involvement can happen in a wide spectrum, involving lacrimal glands, conjunctiva and fornices, cornea, anterior chamber, and vitreous cavity. We report a case of adult filarial worm (B. malayi) inside a conjunctival granuloma in a lady hailing from a rural, non-endemic part of the country. The lady presented with a short history of ocular irritation and redness. Clinical examination revealed a small granuloma-like lesion with surrounding inflammation over the conjunctiva. The rest of the anterior segment as well as the posterior segment was fairly within normal limits. The history as well as clinical examination was not supportive of a parasitic infestation, leading the doctors to treat the lesion as an allergic disease. However, the lesion remained unresolved, and surgical excision was undertaken. On surgical intervention, a live worm was spotted inside the lesion. Parasitological evaluation of the worm was confirmatory of adult filaria (B. malayi). The patient responded to a combination therapy of oral diethylcarbamazine and albendazole.
Keywords
Ocular filariasis
Wuchereria bancrofti
Brugia malayi
African eye worm
Adult filaria worm in eye
INTRODUCTION
Ocular infestation by filarial worms is infrequent. Intraocular infestation in Brugia and Wuchereria filariasis has been reported in India and Southeast Asia.[1-8] This predominantly lymphatic disease can affect the eyes on rare occasions and has always posed a diagnostic challenge for ophthalmologists, especially in cases of atypical presentations. This vector-borne parasitic disease is caused by nematodes Wuchereria bancrofti and Brugia malayi in India. It is mostly a disease in rural areas transmitted by mosquitoes Mansonia, Anopheles, and Aedes. Domestic animals may act as reservoirs of infection. Patients contract the disease through repeated episodes of mosquito bites, although the exact route of ocular involvement is still unknown. Involvement of the anterior chamber as well as the vitreous cavity by the parasite has been reported. The entry of the worm into the anterior chamber has been presumed to be through ciliary vessels. The ocular manifestations of filariasis are elephantiasis of eyelids, iritis, retinal hemorrhages, and the presence of microfilaria in lacrimal gland secretion.[1,2] Loa loa filariasis (Loiasis) transmitted by African eye worms by flies of the genus Chrysops is a disease of submucosal and subcutaneous tissues. L. loa filariasis is endemic in Central and West Africa. Eye worms are a pathognomonic finding of the disease, and adult worms can be visualized migrating in the bulbar sub-conjunctival space, causing irritation and inflammation.[3,4,7] The microfilaria matures into the third larval stage within the fly and enters a human host through subsequent blood meals, where the larva matures into adult forms.[3,4,7] We report a case of a live adult filarial worm inside a conjunctival granuloma, which was initially mistaken as an allergic inflammation. The patient was operated on for excision of granuloma and the live worm was found inside the lesion during surgery.
CASE REPORT
A 50-year-old lady, a homemaker from rural Assam, presented with complaints of irritation and redness in her right eye for 1 month. There was a history of something falling over her eye a few days back while traveling. She had no contact with pets or cattle. On examination, vision in both her eyes was 20/20. There was a small granuloma-like conjunctival lesion in her right eye with localized inflammation [Figure 1] and the rest of the anterior segment was within normal limits. The posterior segment of the right eye showed no abnormality. We prescribed topical steroids (loteprednol etabonate 0.5%) in tapering dosage for 1 month. The patient reported to us after 1 month of applying topical medications, but the lesion remained the same as before, with some decrease in the inflammation. We planned for surgical excision and biopsy of the lesion. Intraoperatively, after placing an incision over the lesion, a slender, long, whitish worm-like organism was seen wriggling out of the lesion [Figure 2]. The live worm was removed, and the wall of the lesion was excised. The organism was sent for parasitological evaluation in normal saline. Postoperatively, the patient was started on oral albendazole (400 mg) weekly dose. Ultrasonography B scan and ultrasound biomicroscopy of the right eye were done to rule out the involvement of vitreous and anterior chamber angles of the eye. Routine blood investigations showed eosinophilia. There was no evidence of microfilaria in peripheral blood examination. Naked eye examination of the organism showed a whitish color slender worm, which measured 42.4 mm in length and 0.5 mm in thickness. Under the light microscope, the worm was identified as a nematode with a blunt cephalic and a tapering caudal end with surface striations. There was a long double-walled tube with a lumen [Figure 3a]. The nematode was diagnosed as an adult-stage filarial worm, most likely to be B. malayi. The cyst wall showed microscopic features of pyogenic granuloma [Figure 3b]. The patient was started on diethylcarbamazine (DEC). She responded well to a combination therapy of albendazole and DEC.
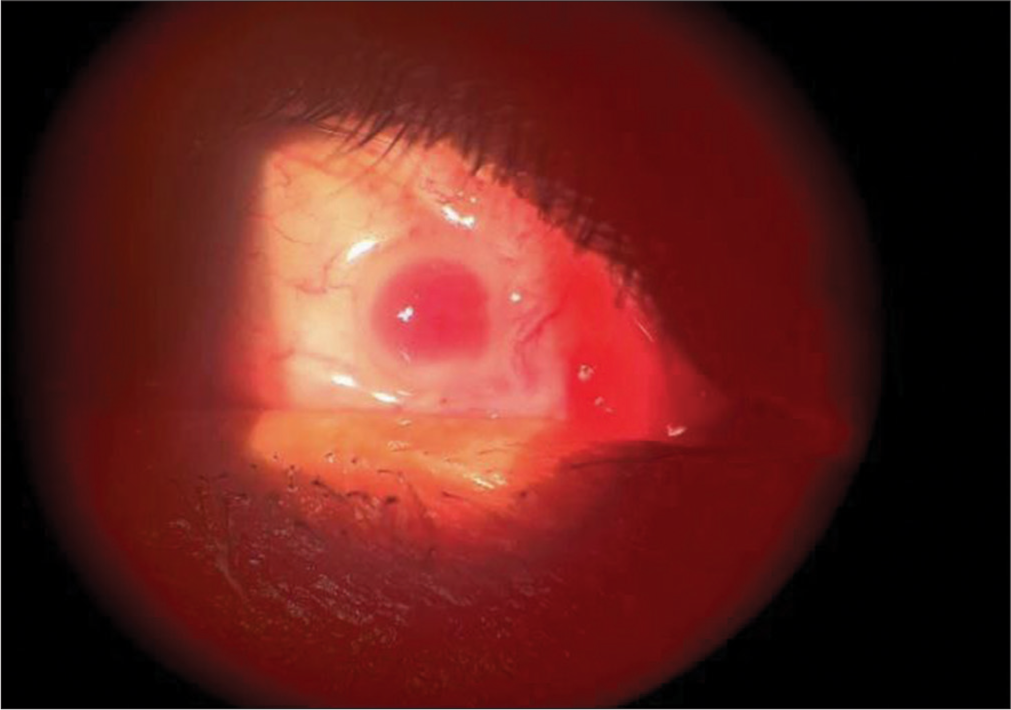
- Slit lamp photography showing conjunctival granuloma with surrounding inflammation.
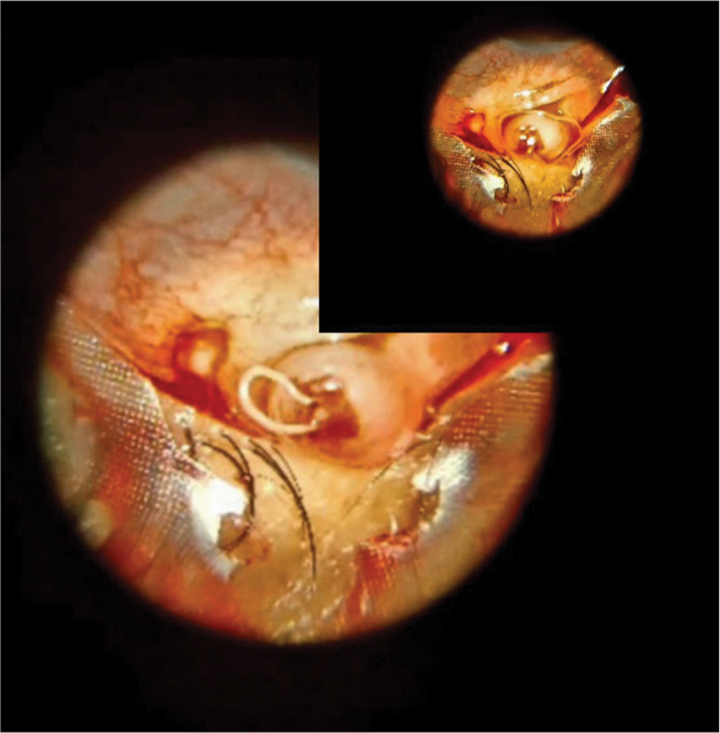
- Montage of intraoperative image of live filarial worm wriggling out.
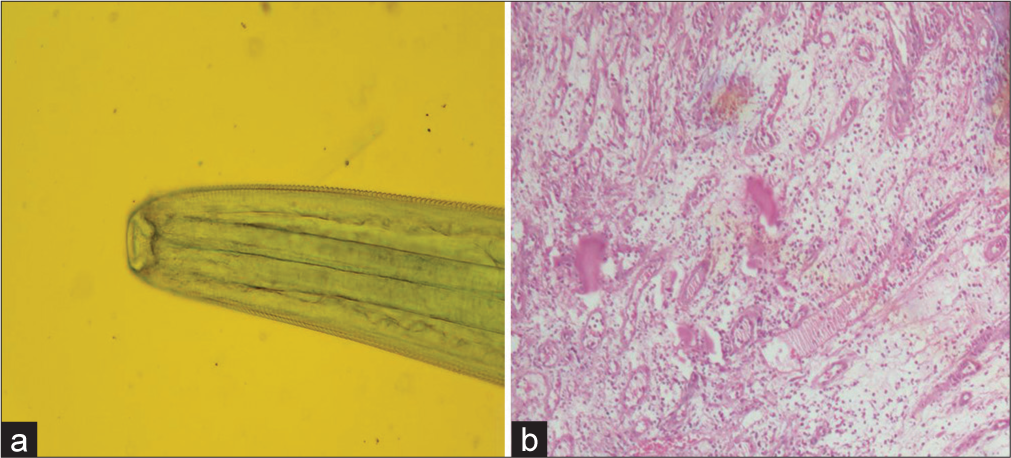
- (a) Microphotograph of wet mount preparation of the head end of the parasite with surface striations in fluorescein stain (×40). (b) Microphotograph of Hematoxylin and Eosin stained section showing proliferation of vascular channels with inflammatory cells (×20).
DISCUSSION
B. malayi is a helminth belonging to the class nematode. Man is the definitive host and Anopheles mosquitoes are the intermediate hosts. Adult filarial worms are thread-like structures that live in the subcutaneous tissue and the lymphatic system, discharging live embryos (microfilaria) into the bloodstream. They sexually reproduce microfilaria, the first larval stage, which is ingested by the hematophagous arthropods, developing into infective larvae that grow in the vertebrate host and mature into adult worms. The route of ocular invasion is still indefinite, with long and short posterior ciliary vessels, cerebrospinal fluid, or the optic nerve sheath being the possible routes of entry inside the eye. Intraocular filariasis is more commonly known to be caused by microfilaria than by adult worms. W. bancrofti and B. malayi are the main causative organisms of intraocular filariasis in India. Ocular filariasis is reported as a rare incidence in endemic and non-endemic parts of the country. The presence of the worm inside the eye usually remains unnoticed in the early phase and is discovered as an incidental finding or when ocular inflammation and related symptoms have already set in. The microfilariae cause uveitis secondary to intraocular filariasis in the Indian subcontinent. The presence of live worms in the anterior chamber causing iritis has been documented in a few reports.[1,2] Corneal edema due to intraocular dead worms as well as live filarial worms in the anterior chamber has been reported.[8] The presence of worms in the vitreous cavity-causing intraocular inflammation has also been documented. The worm can migrate to various parts of the eye, causing structural damage and severe intraocular inflammation. Intact removal of live worms is therefore essential not only for the proper identification of organisms but also to reduce the chances of severe intraocular inflammation from lysed worms. African filarial worm (L. loa), which is endemic in the African rainforest areas, is transmitted by Chrysops fly, which has daily activity and is ingested during a blood meal. L. loa is usually restricted to African rainforests. Sporadic occurrences of this worm in India have been recorded and are extremely rare.[7] Literature also suggests evidence of L. Loa filariasis in Western countries in immigrants and travelers where eye worm migration had been found equally in travelers and African immigrants irrespective of their microfilaremia status.[6] Adult worms are found migrating in the sub-conjunctival space. Incidences of worms in the anterior chamber have also been reported.[3-6]
In our case, the absence of any definite history and the fact that the patient belongs to a non-endemic zone did not lead us to suspect the possibility of parasitic infestation. Moreover, the presence of conjunctival granuloma in the absence of anterior chamber reaction or vitreous involvement was not usual for B. malayi filariasis.
CONCLUSION
Occasionally, familiar lesions,such as a conjunctival granuloma, can have unfamiliar findings. Therefore, common lesions that are not responding to conventional management should intrigue the presence of an unidentified causative factor. Ocular filariasis can happen in the form of conjunctival granuloma or sub-conjunctival live worm. The nematode can also be found in the anterior chamber and vitreous cavity in dead or living form, resulting in corneal edema and severe intraocular inflammation. Prompt and intact removal of live worms is essential to prevent ocular catastrophes.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ocular filariasis: Dancing sensation in the anterior chamber. Trop Parasitol. 2019;9:57-8.
- [Google Scholar]
- Localization of the filaria Loa loa in the anterior chamber of the eye. Acta Trop. 1984;41:265-9.
- [Google Scholar]
- Removal of worm (Filaria Loa) from the eye. Br Med J. 1918;1:502-4.
- [CrossRef] [PubMed] [Google Scholar]
- L'odyss'ee d'une filaire Loa-Loa. A ptopos d'une observation de Filariose sous-conjonctivale [The odyssey of a loa-loa filaria. Apropos of a case of subconjunctioval filariasis. Bull Soc Ophtalmol Fr. 1064;64:927-9.
- [Google Scholar]
- Imported Loa loa filariasis: Three cases and a review of cases reported in non-endemic countries in the past 25 years. Int J Infect Dis. 2012;16:e649-62.
- [CrossRef] [PubMed] [Google Scholar]
- Presence of adult Loa loa in the anterior chamber of the eye along with microfilaremia from non-endemic region: A rare presentation from India. Tzu Chi Med J. 2019;31:283-5.
- [CrossRef] [PubMed] [Google Scholar]
- Persistent corneal edema secondary to presumed dead adult filarial worm in the anterior chamber. Indian J Ophthalmol. 2007;55:67-9.
- [CrossRef] [PubMed] [Google Scholar]






