Translate this page into:
Outcome of Descemet membrane detachment repair using air descemetopexy and Descemet membrane suturing after cataract surgery

*Corresponding author: Parmita Dutta, Department of Cornea, Sri Sankaradeva Nethralaya, Guwahati, Assam, India. parmitadutta0@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Das DR, Dutta P, Agarwal B, Bhattacharjee H. Outcome of Descemet membrane detachment repair using air descemetopexy and Descemet membrane suturing after cataract surgery. Lat Am J Ophthalmol. 2024;7:5. doi: 10.25259/LAJO_27_2023
Abstract
This case series aimed to determine the outcomes of Descemet membrane detachment (DMD) repair after cataract surgery using air descemetopexy, Descemet membrane (DM) suturing, or a combination of these techniques. In this retrospective, interventional case series, the medical records of six patients who underwent DM repair performed by a single surgeon after cataract surgery between February 2022 and February 2023 was obtained from the hospital. Slit-lamp grading of DMD was mild, moderate, or severe. Anterior segment optical coherence tomography (AS-OCT) was performed for patients with diffuse corneal edema. Air descemetopexy and DM suturing were performed according to standard treatment guidelines. The anatomical, functional, and clinical outcomes were assessed. Four patients had DM reattachment, and one patient had persistent DMD that led to the decompensated cornea that underwent Descemet’s stripping endothelial keratoplasty (DSEK). Four patients had best-corrected visual acuity (BCVA) <logMAR 0.3 at 4–6 weeks of follow-up, and two had BCVA >logMAR 0.3. Clinical outcomes showed a clear cornea in four patients, a decompensated cornea in one patient, and a scarred cornea in one patient. In moderate and severe DMD cases, prompt and adequate surgical intervention in the form of air descemetopexy and DM suturing reduces the rate of corneal transplantation.
Keywords
Descemet membrane detachment
Air descemetopexy
Descemet membrane suturing
INTRODUCTION
The Descemet membrane (DM) is 7-micron thick and is composed of type 4 collagen and laminin. It is elastic and curls upon being severed.[1] DM can detach from the posterior corneal stroma during different eye surgeries, including cataract surgery, leading to vision-threatening corneal decompensation.[2] The incidence noted after cataract surgery is very low: Extracapsular cataract extraction, 0.26%; manual small incision cataract surgery (SICS), 0.1% and phacoemulsification, 0.04%.[3]
Slit-lamp grading of Descemet membrane detachment (DMD) was classified as mild (<25% of the cornea and periphery), moderate (25–50% of the cornea and periphery), and severe (>50% of the cornea or involved central cornea). DMD can be classified as planar (when separation from the posterior stroma is ≤1 mm), and non-planar (when separation from the posterior stroma is >1 mm).[4]
The anterior segment optical coherence tomography (AS-OCT) grading of DMD was defined as simple detachment (the DM showed local detachment involving <1/4 of the corneal area), symmetrical detachment (1/4–1/2 of the detached corneal area), and complete detachment (>1/2 of the detached corneal area).[5]
Here, we report a case series of six cases of DMD that occurred after cataract surgery and their management by air descemetopexy and DM suturing. We analyzed different approaches for each case and their respective outcomes.
MATERIAL AND METHODS
Data was collected from hospital medical records. Approval was obtained from the Institutional Review Board and the Ethical Committee. This case series was conducted in accordance with the tenets of the Declaration of Helsinki.
Written informed consent was obtained from the patients for the images and clinical information to be reported.
This retrospective and interventional case series reviewed the outcomes of six patients who underwent surgical repair of DMD after cataract surgery by a single surgeon from February 2022 to February 2023.
Preintervention evaluation
DMD was diagnosed using slit-lamp examination (SLE) of the cornea outpatient department.
AS-OCT was performed only for severely edematous corneas.
Slit-lamp grading of DMD was performed. The characteristic features of DMD include extent, location (central or peripheral), planar or non-planar, and corneal edema.[6]
Surgical intervention technique
Air descemetopexy
All interventions were performed under peribulbar anesthesia in the operation theater. Paracentesis was performed in an area with attached DM. Air was injected, and a 2-cc syringe was used to unscroll and reattach the DM to the posterior stroma. The anterior chamber (AC) was filled with air, and the patients were maintained in a supine position after which partial release of air was done to fill only 2/3rd of the AC. The patients were placed in a strict supine position during the immediate post-operative period.[3]
DM suturing
DM suturing was performed under local anesthesia. Full-thickness interrupted sutures with 10-0 nylon sutures were placed in the mid-peripheral portion of the cornea tangential to the limbus. The suture bite was directed from the area of the attached DM to that of the detached DM. AC was formed with air.[4]
Functional outcome was defined as best-corrected visual acuity (BCVA) at 3–6 months. The anatomical outcome was defined as reattachment of the detached DM, as noted on SLE. The clinical outcome was defined as a clear cornea or persistent corneal edema.
RESULTS
Case 1
A 65-year-old woman underwent SICS of the right eye (OD). On post-operative day 1 (POD 1), the vision was logMAR 0.7, and the cornea revealed diffuse stromal edema on SLE. The patient was advised of post-operative medications. Two weeks later, SLE revealed a non-planar central DMD covering up to 50% of the cornea. She underwent air descemetopexy and full-thickness suturing of the central cornea on day 15. POD 1 vision was logMAR 1 which improved to logMAR 0 at 10 days. On SLE, the DM was completely attached, with a clear cornea.
Case 2
A 65-year-old woman underwent SICS in the left eye (OS). Her vision on POD 1 was counting fingers close to face (CFCF) with diffuse corneal edema on SLE. She was advised post-operative medications and was asked to review them after one week. After two weeks, localized non-planar DMD was observed in the superonasal and inferior quadrants. Full-thickness DM suturing was performed. POD 1 vision was logMAR 0.7. However, after five days, the DM was curled with corneal edema. The patient was scheduled to undergo Descemet stripping endothelial keratoplasty (DSEK).
Case 3
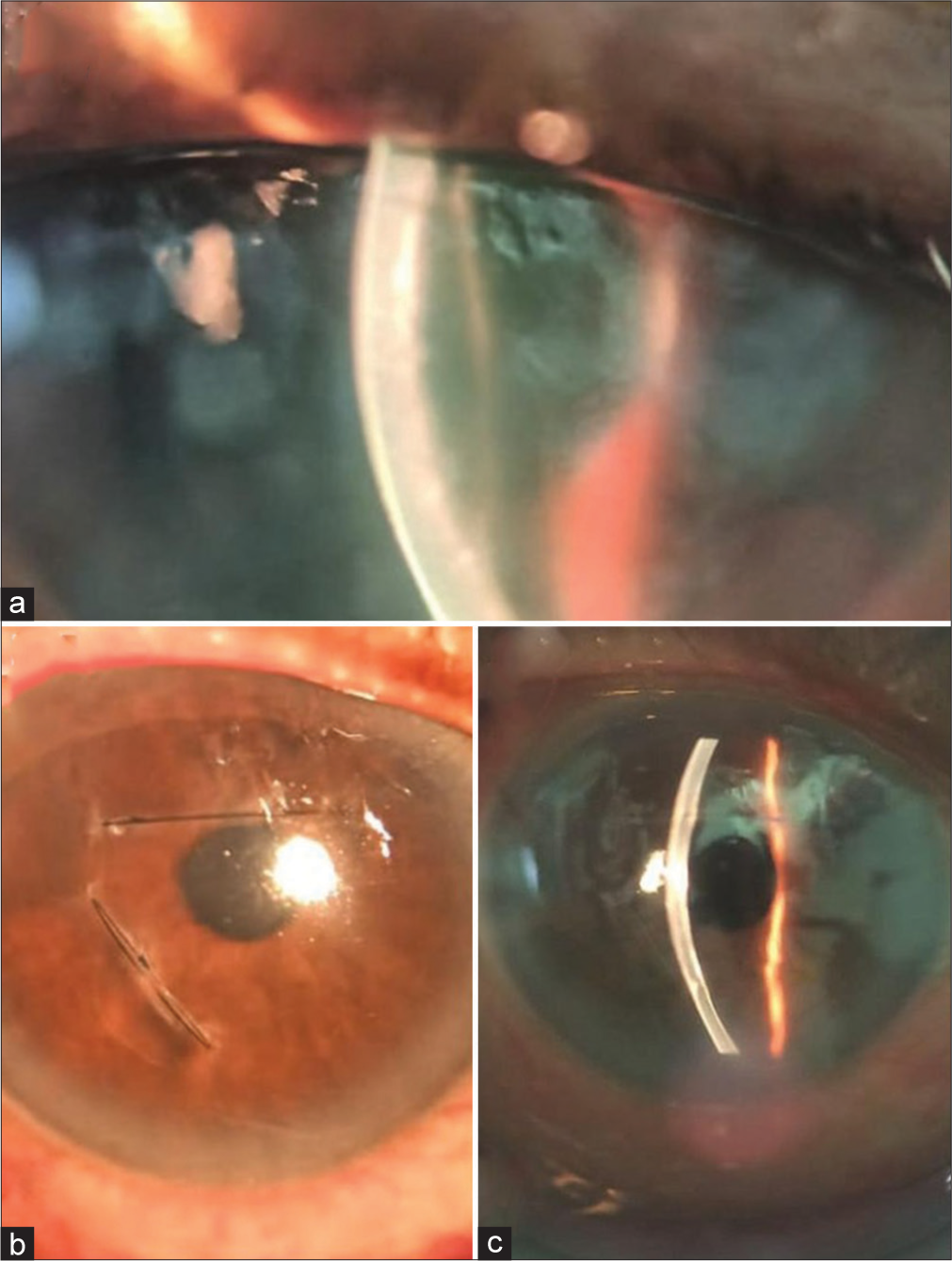
A 54-year-old woman underwent SICS in the right eye. On POD 1, vision was logMAR 0.3, and SLE revealed corneal edema in the central and inferior parts [Figure 1] with non-planar DMD on day. She was advised to undergo DMD repair on day 5. However, the patient was lost to follow-up and was reviewed after 1 month. Air descemetopexy was performed. POD 1 vision was logMAR 0.3, cornea was clear with 50% air bubble in situ. After a month, BCVA improved to logMAR 0, and her DM was reattached on SLE.

- Pre-operative and post-operative images (a) Postoperative image showing clear cornea and air bubble in situ (b) Pre-operative image showing diffuse corneal edema (c) Pre-operative image showing non-planar Descemet membrane detachment.
Case 4
A 70-year-old man underwent phacoemulsification surgery in his right eye and was referred to us 25 days after his initial surgery. On SLE, he was found to have corneal edema and non-planar DMD [Figure 2]. Air descemetopexy was performed on day 27; however, residual DMD was observed on the 2nd day. The patient underwent repeat surgery with two,full-thickness corneal sutures and a 70% air bubble. Vision on POD 1 was logMAR 0.3 with 70% air bubble in situ. One month later, the DMD was completely reattached [Figure 3], and the patient’s BCVA was logMAR 0.2. At the 9-month follow-up, BCVA remained the same, with localized scarring of the DM away from the visual axis.
- Pre-operative and post-operative image (a) pre-operative image showing non-planar Descemet membrane (DM) detachment (b) Post-operative image showing corneal sutures placed in the superior half and mid periphery temporally (c) Post-operative slit-lamp image showing attached DM.
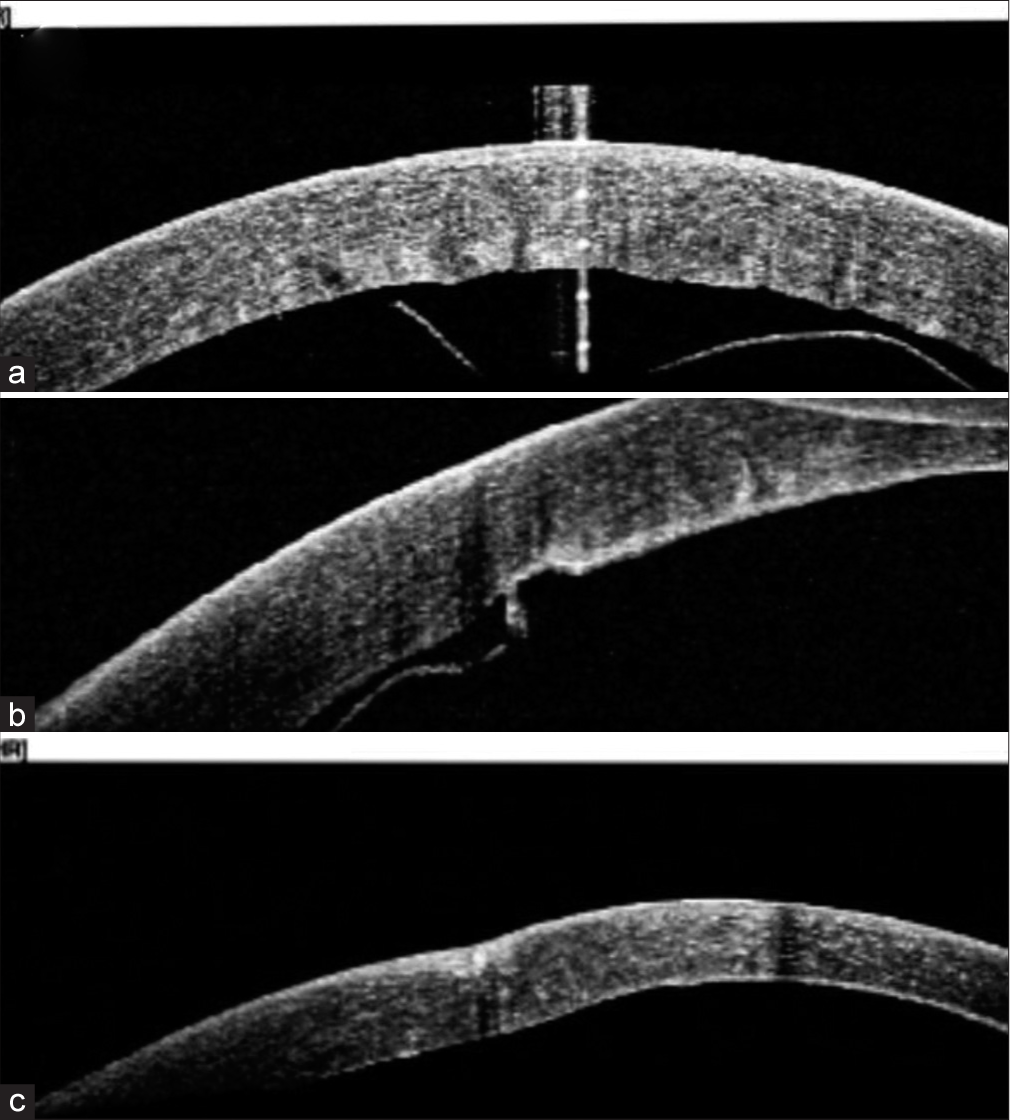
- Anterior segment optical coherence tomography (ASOCT) images (a) pre-operative AS-OCT image showing central curled up Descemet membrane (DM) detachment (b) Postoperative day 1 AS-OCT image showing inferior residual detachment (c) Post-operative AS-OCT image at 1 month showing attached DM.
Case 5
A 60-year-old man underwent phacoemulsification of OD. On POD 1, SLE revealed localized stromal edema superiorly with planar DMD [Figure 4]. On day 5, the patient underwent air descemetopexy. POD 1 vision was logMAR 0.7; the cornea was clear. After one month, the patient’s BCVA was logMAR 0.3 with a clear cornea and complete DM attachment.
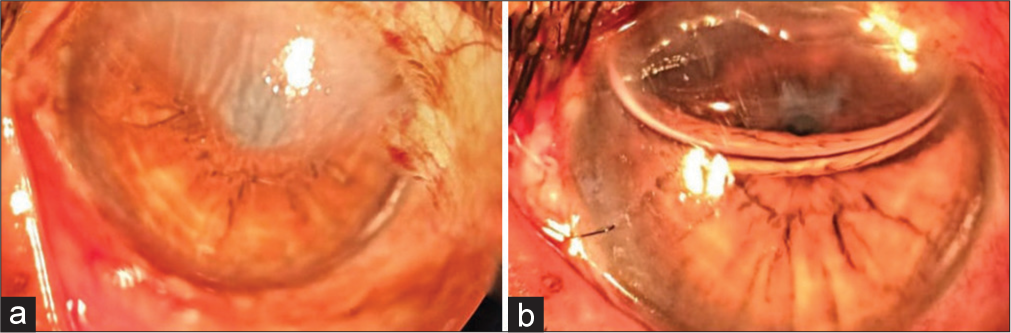
- Pre-operative and post-operative images (a) pre-operative slit-lamp image showing corneal edema in the superior part and (b) post-operative image showing clear cornea and air bubble in situ
Case 6
A 60-year-old woman underwent SICS for OS. Intraoperatively, the patient had a central DMD that was reattached using air descemetopexy. On POD 1, the vision was CFCF, with mild corneal edema, an attached DM and 70% air bubble in situ. Fundus examination revealed retinal pigment epithelial (RPE) alterations in the fovea. After three days, BCVA improved to logMAR 1.
All six cases were successfully managed using air descemetopexy and/or DM suturing, except case 2, which required DSEK due to corneal edema, intraoperative DM loss, and endothelial cell loss. All patients were followed up regularly.
DISCUSSION
DMD management includes hyperosmotics and topical steroids for smaller, shallower detachments. For larger, deeper, central detachments, tamponade with air or isoexpansile gasses, such as C3F8, and SF6 may be used to reattach the DM. Corneal suturing was performed in cases of larger, centrally scrolled DMD.[2,7]
Our case series focused on moderate-to-severe DMD. The incidence of DMD was higher after SICS.[2,3]
The patient’s demographic characteristics, pre-operative findings, interventions, and post-operative data are shown in Table 1.
| Age in years/sex | Eye | Pre-operative VA | Time to repair | Grading of DMD/intervention used | Post-operative clinical outcome at final follow-up | Post-operative functional outcome | Post-operative anatomical outcome (Reattachment of DM) | Ocular comorbidity affecting vision | |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | 65 /F | OD | Logmar 1.8 | Day 14 | Severe, NP/Air Dpexy+DM suturing | Clear cornea (on day 10) | ≤logMAR 0.3 | Yes | |
| Case 2 | 65/F | OS | Logmar 1.8 | Day 15 | Severe, NP/DM suturing | Decompensated cornea | >logMAR 0.3 | No | Hypertensive retinopathy |
| Case 3 | 54/F | OS | Logmar 0.3 | Day 36 | Severe, NP/Air D pexy | Clear cornea (on day 3) | ≤logMAR 0.3 | Yes | |
| Case 4 | 70/M | OD | Logmar 1.48 | Day 27 | Severe, NP/Air D pexy+DM suturing | Scarred cornea (at 9 months) | ≤logMAR 0.3 | Yes | |
| Case 5 | 60/M | OD | LogMAR 1 | Day 5 | Moderate, Planar/Air Dpexy | Clear cornea (on day 3) | ≤logMAR 0.3 | Yes | Lagophthalmos |
| Case 6 | 60/F | OS | CFCF | Day 0 | Moderate, planar/Air D pexy | Clear cornea (on day 3) | >logMAR 0.3 | Yes | Retinal pigment epithelium alterations |
OD: Right eye, OS: Left eye, VA: Visual acuity, CFCF: Counting fingers close to face, NP: Non-planar, D pexy: Descemetopexy, DMD: Descemet membrane detachment, DM: Descemet membrane
In our case series, clinical outcomes showed clear cornea in 4 (67%) patients, decompensated cornea in 1 (33%) patient, and scarred cornea in 1 (33%) patient [Table 1]. Das et al., in 2019, showed clear cornea in 85% of cases and corneal decompensation in 14% of cases.[2]
Anatomical outcomes in our case series showed DM reattachment in 4 cases (67%) and persistent DMD in 1 (16%) [Table 1]. In their study, Chaurasia et al. showed DM reattachment in 13 cases, and persistent DMD in one case.[8]
In our case series, functional outcomes were taken at 3–6 months duration. Four patients had BCVA ≥logMAR 0.3, and two patients’ BCVA was <logMAR 0.3 (Case 2 and Case 6) [Table 1]. Case 2 had persistent DMD, and Case 6 had RPE alterations in the fovea.
In our case series, all patients were started on hyperosmotic and topical dexamethasone in tapered doses postoperatively until the intervention except in Case 4 which presented to us on day 25 of surgery.
Huang HC et al., in 2020, concluded that 20% SF6 descemetopexy was good for anatomical outcomes but caused increased intraocular pressure (IOP) postoperatively due to pupillary block, requiring additional peripheral iridectomy.[6] In addition, long-term tamponade has deleterious toxic effects on corneal endothelium. However, in our case series, air descemetopexy was found to have good clinical, anatomical, and functional outcomes with no risk of increased IOP and corneal endothelial toxicity.
The limitations of our case series are as follows:
Small case series
Long-term follow-up could not be documented
AS-OCT and specular microscopy could not be performed as the majority of them received treatment from the non-paying section.
Nevertheless, meticulous clinical examination and prompt surgical intervention can result in good anatomical and functional outcomes, as seen in our case series.
CONCLUSION
In moderate and severe DMD cases, prompt and adequate surgical intervention by air descemetopexy, DM suturing, or a combination of these methods helps maintain corneal clarity and reduces the rate of corneal transplantation in the future.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anatomy of cornea and ocular surface. Indian J Ophthalmol. 2018;66:190.
- [CrossRef] [PubMed] [Google Scholar]
- Descemet membrane suturing for large Descemet membrane detachment after cataract surgery. Cornea. 2020;39:52-5.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective study on the incidence of post-cataract surgery Descemet's membrane detachment and outcome of air descemetopexy. Br J Ophthalmol. 2018;102:182-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic and visual outcomes of descemetopexy in post-cataract surgery Descemet's membrane detachment. Ophthalmology. 2013;120:1366-72.
- [CrossRef] [PubMed] [Google Scholar]
- Study on the classification of Descemet membrane detachment after cataract surgery with AS-OCT. Int J Med Sci. 2018;15:1092.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Descemet's membrane detachment after cataract surgery-a case series. Reports. 2020;3:13.
- [CrossRef] [Google Scholar]
- Outcomes of descemetopexy with isoexpansile perfluoropropane after cataract surgery. J Ophthalmic Vis Res. 2016;11:168-73.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of air descemetopexy for Descemet membrane detachment after cataract surgery. J Cataract Refract Surg. 2012;38:1134-9.
- [CrossRef] [PubMed] [Google Scholar]







