Translate this page into:
Outcome of intense-pulsed light therapy versus combination of intense-pulsed light and low-level light therapy for the treatment of meibomian gland dysfunction

*Corresponding author: Parmita Dutta, Department of Cornea, Sri Sankaradeva Nethralaya, Guwahati, Assam, India. parmitadutta0@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agarwal B, Dutta P, Kalita S, Das DR, Singh A. Outcome of intense-pulsed light therapy versus combination of intense-pulsed light and low-level light therapy for the treatment of meibomian gland dysfunction. Lat Am J Ophthalmol. 2024;7:3. doi: 10.25259/LAJO_4_2024
Abstract
Objectives:
The objective of this study was to study the efficacy of intense pulsed light (IPL) therapy and a combination of intense pulse light therapy and low-level light therapy (LLLT) in treating meibomian gland dysfunction (MGD).
Material and Methods:
In this prospective and hospital-based interventional study, 32 patients were enrolled between April 2023 and January 2024 in the Department of Cornea, Sri Sankaradeva Nethralaya, Guwahati. The clinical evaluation was done included the ocular surface disease index (OSDI-6) questionnaire score, tear film break-up time (TBUT), Schirmer test I, slit-lamp examination for lid evaluation to see signs of pitting, telangiectasia, meibomian gland expressibility, meibography (to see gland dropout assessment), and meibomian gland loss percentage (MGL%). The enrolled participants were randomly allocated to receive IPL and combination light therapy (IPL+LLLT) in a 1:1 ratio.
Results:
Sixty-two eyes of 31 patients were included in this study. In the IPL group, the level of dryness (LOD) improved in nine (56.25%) cases and remained the same in seven cases (73.75%). In the IPL+ LLLT group, the LOD improved in eight cases (53.3%) and remained the same in six (40%) cases. For the right eye (OD), the MGL% was 0.46 ± 0.08 at baseline, which decreased to 0.32 ± 0.07 at six months. For the left eye (OS), MGL% was 0.52 ± 0.09 at baseline, and at six months, it reduced to 0.34 ± 0.08. In OD, MGL% was 0.46 ± 0.06 at baseline, reduced to 0.35 ± 0.12 at six months. In OS, MGL% was 0.49 ± 0.09 at baseline, and at six months, it reduced to 0.35 ± 0.12. In the IPL group, the mean TBUT in OD improved from 3.25 to 5.25 in 1 month. The mean TBUT for OS improved from 4.19 to 6.44 in OS. In the IPL+LLLT group, the mean TBUT in OD improved from 3.2 to 5.2 at one month in OS. The mean TBUT in OS improved from 4.27 to 6 in one month.
Conclusion:
IPL alone or in combination with LLLT has similar efficacy in treating MGD. There was a reduction in the OSDI score LOD with improved TBUT and decreased MGL% at the end of 1, and six months.
Keywords
Intense-pulsed light
Meibomian gland dysfunction
Low-level light therapy
INTRODUCTION
The global prevalence of dry eye disease lies between 50% and 80.4%, with a large majority showing signs of meibomian gland dysfunction (MGD).[1] MGD is a type of posterior blepharitis. It is a condition of meibomian gland obstruction secondary to hyperkeratinization of the duct epithelium or plugging with a solidified secretion. It is the most common cause of evaporative dry eye.[2] Symptoms of MGD are non-specific and include burning, itching, red eyes, and decreased or fluctuating vision. The lid margin is often rounded with thickening, erythema, hyperkeratinization, vascularization, telangiectasia, or notching.[3]
The degree of MGD can be graded on a meiboscale as degree 0 (0% meibomian gland loss in the lower tarsal area), degree 1 (<25% meibomian gland loss in the lower tarsal area), degree 2 (25–50% meibomian gland loss in the lower tarsal area), degree 3 (51–75% meibomian gland loss in the lower tarsal area), and degree 4 (>75% meibomian gland loss in the lower tarsal area).[4]
Conventional treatment of MGD involves the application of warm compresses followed by lid margin massage to restore the normal release of meibum lipids into the tear film. In recent years, novel devices have emerged to allow in-office MGD management, including intense-pulsed light (IPL), which is based on a polychromatic light source with a wavelength spectrum of 500–1200 nm, which is directed to the periocular skin. The thermal effect on the irradiated tissue leads to the ablation of blood vessels and liquefaction of the meibum.[5]
Low-level light therapy (LLLT) is a new technology that uses near-infrared light to elicit mitochondrial light absorption and induce cell photoactivation with changes in inflammatory protein expression. LLLT has been used for MGD, and devices that allow for combined treatment with IPL and LLLT have become commercially.[5,6]
The eye-light device combines IPL and LLLT. Combined IPL and LLLT may result in softening of the meibum, which relieves obstruction of the glands, and stimulation of the glands.[7]
This study compared the efficacy of IPL and a combination of IPL and LLLT in the treatment of MGD.
MATERIAL AND METHODS
Study design and ethical approval
Approval was obtained from the Institutional Review Board and Ethical Committee before conducting this study.
Written informed consent was obtained from the patients for their images and other clinical information to be reported in the journal.
Compliance with the STROBE checklist has been maintained in this manuscript.
This single-center and prospective study was conducted in Sri Sankaradeva Nethralaya, Guwahati, India, from April 2023 to January 2024. This study adhered to the tenets of the Declaration of Helsinki.
Patients attending the cornea and ocular surface outpatient department during this period were screened for allotment.
The inclusion criteria were as follows:
Age ≥18 years,
Subjects with clinical diagnosis of MGD
Meiboscore grade 3 and above.
Exclusion criteria were as follows:
Previous ocular surgery,
Use of hypotensive eye drops
Contact lens wearers
Skin pigmented lesions in the treatment areas,
Pregnancy and breastfeeding, and
Inability to comply with the treatment or with follow-up.
Detailed history regarding age, sex of the participant, onset, duration, and type of symptoms and presence of any ocular and systemic comorbidities were recorded. The enrolled participants were randomly allocated to receive IPL and combination light therapy (IPL+LLLT) in a 1:1 ratio.
Intervention
All treatments were conducted using the eye-light device (Espansione Marketing S.p.A., Bologna, Italy) and the MY MASK-E (Espansione Marketing S.p.A., Bologna, Italy) for IPL and LLLT, respectively. For IPL treatment, skin in the areas to be treated was cleaned. Hyperpigmented skin lesions were covered with a protective adhesive. The level of energy delivered was automatically set for each patient according to the Fitzpatrick skin pigmentation grading scale and the manufacturer’s recommendations. Protective eye shields were placed on the patient’s eyes. The person who applied the treatment had protective goggles. Five IPL pulses were applied to each eye (three perpendiculars to the inferior orbital rim, one at the lateral canthus, and one applied horizontally along the inferior orbital rim). In patients in the IPL+LLLT group, IPL treatment was followed by bilateral LLLT for 15 min. No eye shields were used for this treatment; the LLLT mask was applied, and the patients were instructed to keep their eyes closed to ensure complete treatment of the upper and lower eyelids.[8,9]
Ophthalmic evaluations were performed at baseline. Uncorrected visual acuity and best corrected visual acuity bcva were assessed. The ocular surface disease index (OSDI) questionnaire was used to assess ocular surface discomfort. Tear film break-up time (TBUT) and Schirmer’s test were recorded. Meiboscore and meibomian gland loss percentage (MGL%) was assessed using the me-check device (Espansione Marketing S.p.A., Bologna, Italy).
The patients were called for follow-up at 1, 3, and 6 months.
Conservative treatment in the form of sodium hyaluronate, loteprednol, moxifloxacin eye drops, azithromycin 1% eye ointment, oral doxycycline 100 mg twice daily for two weeks followed by once daily for one month, and hydroxypropyl methylcellulose eye ointment was administered to every patient.
Statistical analysis
Continuous variables were expressed as mean, median and standard deviation and compared across the groups using the Mann–Whitney U--test because the data did not follow a normal distribution.
Categorical variables are expressed as a number of patients and percentage of patients and compared across the groups using Pearson’s Chi-square test for independence of attributes/Fisher’s Exact Test, as appropriate.
The statistical software Statistical Package for the Social Sciences version 25 was used for the analysis.
An alpha level of 5% was considered significant if P < 0.05.
RESULTS
Demographic data
A total of 64 eyes of 32 patients were included in the study. However, one patient in the IPL+ LLLT group was lost to follow-up during the post-treatment period. Therefore, 62 eyes of 31 patients were considered.
The mean age in the IPL group was 46.6, and the mean age in the IPL+LLLT group was 49.67 [Table 1].
| Group I (IPL) II (IPL+LLLT) | Baseline Mean | Group comparison P-value | |
|---|---|---|---|
| Age | I, II | 46.6, 49.67 | 0.527 |
| Sex (M/F) | I, II | 5/11, 7/8 | 0.379 |
| Thyroiditis | I, II | 4 (12.9%), 0 | |
| Diabetes mellitus | I, II | 0, 2 (6.45%) | |
| Systemic arterial Hypertension | I, II | 2 (12.5%), 1 (6.66%) | |
| Arthritis | I, II | 1 (6.25%), 1 (6.66%) |
IPL: Intense pulse light, LLLT: Low-level light therapy
Twelve (38.71%) patients were male, and 19 (61.29%) were female.
Systemic factors
Four (12.9%) patients had thyroiditis, 3 (9.67%) had systemic arterial hypertension, 2 (6.45%) had diabetes mellitus, 2 (6.45%) had arthritis, 1 (3.22%) had asthma, and 19 patients had no comorbidities [Table 1].
Clinical outcome
OSDI score level of dryness (LOD)
In the IPL group, OSDI score LOD at one month improved in seven cases (43.75%) and remained the same in nine cases (56.25%) [Figure 1].

- Graph showing ocular surface disease index score level of dryness (OSDI) in intense pulse light (IPL) group.
At three months, the OSDI score LOD improved in 8 cases (50%), remained the same in 6 cases (37.5%), and worsened in 2 cases (12.55%).
At six months, the OSDI score LOD improved in nine cases (56.25%) and remained the same in seven cases (43.75%).
In the IPL+LLLT group, OSDI score LOD at one month improved in 5 cases (33.3%) and remained the same in 10 cases (66.6%) [Figure 2].

- Graph showing ocular surface disease index score level of dryness (OSDI) in the intense pulse light (IPL) + low-level light therapy group (LLLT).
At three months, OSDI score LOD improved in 8 cases (53.3%) remained the same in 6 cases (40%), and worsened in 1 case (6.66%).
At six months, OSDI score LOD improved in 8 cases (53.3%), remained the same in 6 cases (40%) and worsened in 1 case (6.66%).
MGL%
In the IPL group
For the right eye (OD), the MGL% was 0.46 ± 0.08 at baseline, that decreased to 0.42 ± 0.09 at one month (P = 0.6), 0.37 ± 0.07 (P = 0.9) at three months, and 0.32 ± 0.07 at six months (P = 0.4) [Table 2].
| MGL% | IPL | IPL+LLLT | P-value |
|---|---|---|---|
| OD | |||
| At baseline | 0.46±0.06 | 0.46±0.06 | |
| At 1 month | 0.42±0.09 | 0.41±0.09 | 0.6 |
| At 3 months | 0.37±0.07 | 0.43±0.12 | 0.9 |
| At 6 months | 0.32±0.07 | 0.35±0.12 | 0.4 |
| OS | |||
| At baseline | 0.52±0.09 | 0.49±0.09 | |
| At 1 month | 0.49±0.07 | 0.45±0.11 | 0.9 |
| At 3 months | 0.42±0.07 | 0.43±0.12 | 0.4 |
| At 6 months | 0.34±0.08 | 0.35±0.12 | 0.4 |
MGL%: Meibomian gland loss percentage, IPL: Intense pulse light, LLLT: Low-level light therapy, OD: Right eye, OS: Left eye
For the left eye (OS), MGL% was 0.52 ± 0.09 at baseline, at one month, it reduced to 0.49 ± 0.07 (P = 0.9), at three months, it reduced to 0.42 ± 0.07 (P = 0.4), and at six months, it reduced to 0.34 ± 0.08 (P = 0.4).
In the IPL+LLLT group
In OD, MGL% was 0.46 ± 0.06 at baseline, which decreased to 0.41 ± 0.09% at one month, 0.43 ± 0.12 at three months, and 0.35 ± 0.12 at six months.
In OS, MGL% was 0.49 ± 0.09 at baseline, at one month, it reduced to 0.45 ± 0.11, at three months, it became 0.43 ± 0.12, and at six months, it reduced to 0.35 ± 0.12.
Mean -TBUT
In the IPL group, the mean TBUT in OD improved from 3.25 to 5.25 in one month. The mean TBUT for OS improved from 4.19 to 6.44 in OS (P = 0.7).
In the IPL+LLLT group, the mean TBUT in OD improved from 3.2 to 5.2 at one month in OS. The mean TBUT in OS improved from 4.27 to 6 at one month (P = 0.8) [Table 3 and Figure 3].
| Mean TBUT | IPL | IPL+LLLT | ||
|---|---|---|---|---|
| OD | OS | OD | OS | |
| At baseline | 3.25 | 4.19 | 3.2 | 4.27 |
| At 1 month | 5.25 | 6.44 | 5.2 | 6 |
TBUT: Tear film break-up time, IPL: Intense pulse light, LLLT: Low-level light therapy, OD: Right eye, OS: Left eye
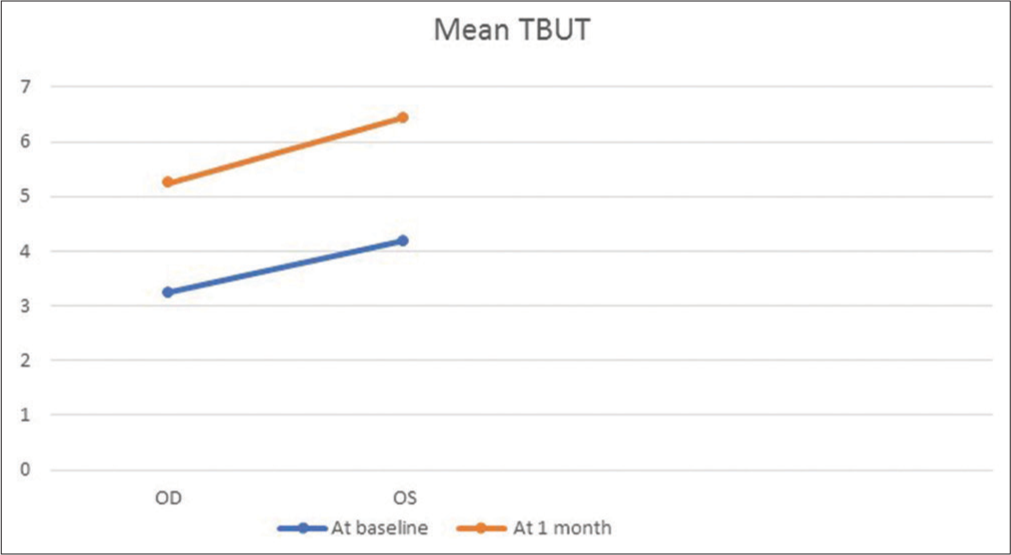
- Graph showing mean tear film break-up time (TBUT). OD : Right eye, OS: Left eye
Repeat setting of IPL
Repeat IPL settings were needed in five patients (31%) and 6 (40%) patients of IPL+LLLT group.
Repeat IPL settings were needed at 1, 1.5, 2, and 6 months. One patient required two sittings at 1 and 2 months [Table 4].
| Intervention | Total | P-value | Significance | ||
|---|---|---|---|---|---|
| IPL | IPL+LLLT | ||||
| Repeat setting needed | |||||
| No | 11 (68.75) | 9 (60) | 20 (64.52) | 0.611 | Not Significant |
| Yes | 5 (31.25) | 6 (40) | 11 (35.48) | ||
| Total | 16 (100) | 15 (100) | 31 (100) | ||
IPL: Intense pulse light, LLLT: Low-level light therapy
Repeat settings of IPL+LLLT were given at 1, 2, and 2.5 months. One patient needed repeat settings at 15 days and one month. The risk of repeat setting in IPL was 1.1 times higher than that in the combination of IPL and LLLT.
No adverse events such as skin burns, blisters or pain, conjunctivitis, skin pigmentation changes, or loss of eyelashes were documented following the procedures.
DISCUSSION
The data presented in our study demonstrate that the OSDI score levels of dryness, TBUT, and MGL% improved in both the IPL and combination (IPL LLLT) groups.
In our study, the male-to-female ratio of the patients was 12:19.
The mean age in our study was 46.6 in the IPL group, and in the IPL+LLLT group was 49.67. The patients in our study were younger than those in the previous studies.[1-3]
In this study, a comprehensive overview of the LOD was performed using the me-check machine.
In the IPL group, dryness improved in 9 cases (56.25%), and in the IPL+LLLT group, dryness improved in 8 cases (53.3%) at the end of 6 months.
The LOD in the IPL group was level 0 at baseline in 7 cases (43.75%), which improved to 11 (68.75%) cases at the end of 6 months (P = 0.5)
The LOD in the IPL+LLLT group was level 0 at baseline in 7 cases (46.6%) which improved to eleven cases (73.3%) at the end of six months (P = 0.3). As indicated by p-value, the changes were not significant.
No previous study has used this parameter to quantify dryness.[9-12]
In the IPL group, thyroid disorder was present in four patients (25%), arthritis in one patient (6.25%), and systemic arterial hypertension in two patients (12.5%).
In the IPL+LLLT group, diabetes was present in two patients (13.3%), arthritis in one patient (6.66%), and systemic arterial hypertension in one patient (6.66%).
This data was comparable with other studies.[10]
In our study, the change in the mean TBUT at one month in the IPL group was 2.25, and that in the IPL+LLLT group was 1.73 (P = 0.8) which was not significant. In the previous study by Stonecipher et al., the change in mean TBUT was 4.4–8 that was significant.[9] Furthermore, other previous studies found significant changes in TBUT after treatment in the combined light therapy (IPL+LLLT) group.[7,11]
In our study, there was a decrease in MGL%, as shown in Table 2. No significant changes were observed in either group of patients. In a study by Marta et al., the MGL% before and after treatment in IPL+LLLT group did not show significant change.[10,12]
To the best of our knowledge, this is the second study that compares one group receiving IPL and the other receiving IPL+LLLT.[12] This is the first study that compares both the aforementioned treatment groups using a single device.[12]
The limitations of the study include the following:
Sample size was small
The OSDI scores were not considered
Due to the use of combined (IPL+LLLT) therapy, it was difficult to identify any benefits of LLLT alone.
CONCLUSION
IPL alone or in combination with LLLT has a similar efficacy in treating MGD. There was a reduction in the OSDI score LOD with improved TBUT and decreased MGL% at the end of 1, 3, and 6 months.
Ethical approval
The research/study approved by the Institutional Review Board at Sri Sankaradeva Nethralaya, Guwahati, number 9680, dated 6/01/2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: A retrospective study. Cornea. 2012;31:472-8.
- [CrossRef] [PubMed] [Google Scholar]
- The definition and classification of dry eye disease: Report of the definition and classification subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5:82-3.
- [CrossRef] [PubMed] [Google Scholar]
- Meibomian gland dysfunction and seborrhea Cornea (3rd ed). China: Mosby Elsevier; 2011. p. :409-10. Ch. 34
- [Google Scholar]
- Low-level light therapy versus intense-pulsed light for the treatment of meibomian gland dysfunction: Preliminary results from a prospective randomized comparative study. Cornea. 2023;42:141-4.
- [CrossRef] [PubMed] [Google Scholar]
- Is light-emitting diode phototherapy (LED-LLLT) really effective? Laser Ther. 2011;20:205-15.
- [CrossRef] [PubMed] [Google Scholar]
- Meibomian gland dysfunction: Intense pulsed light therapy in combination with low-level light therapy as rescue treatment. Medicina (Kaunas). 2021;57:619.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and molecular outcomes after combined intense pulsed light therapy with low-level light therapy in recalcitrant evaporative dry eye disease with meibomian gland dysfunction. Cornea. 2022;41:1080-7.
- [CrossRef] [PubMed] [Google Scholar]
- Combined low level light therapy and intense pulsed light therapy for the treatment of meibomian gland dysfunction. Clin Ophthalmol. 2019;13:993-9.
- [CrossRef] [PubMed] [Google Scholar]
- Intense pulsed plus low-level light therapy in meibomian gland dysfunction. Clin Ophthalmol. 2021;15:2803-11.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of intense pulsed light in patients with meibomian gland dysfunction-a randomized, double-masked, sham-controlled clinical trial. Cornea. 2020;39:325-32.
- [CrossRef] [PubMed] [Google Scholar]
- Low-level light therapy in association with intense pulsed light for meibomian gland dysfunction. Clin Ophthalmol. 2022;16:4003-10.
- [CrossRef] [PubMed] [Google Scholar]







