Translate this page into:
Stereoscopic fundus photograph, optical coherence tomography features, and fundus autofluorescence in a focal combined retinal and choroidal coloboma

*Corresponding author: Victor Andrade de Araújo, Department of Ophthalmology, Hospital Geral de Fortaleza, Fortaleza, Brazil. victoraa77@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: de Araújo VA, Moreira PG, Ferreira BF. Stereoscopic fundus photograph, optical coherence tomography features, and fundus autofluorescence in a focal combined retinal and choroidal coloboma. Lat Am J Ophthalmol. 2024;7:6. doi: 10.25259/LAJO_25_2023
Abstract
Chorioretinal coloboma is a rare condition caused by incomplete closure of the embryonic fissure. We report a case of a 34 years old with a unilateral retinal and choroidal coloboma in the right eye, highlighting the use of stereoscopic fundus photograph, spectral-domain optical coherence tomography, and fundus autofluorescence. Regular eye examinations are crucial to detect changes in patients with a higher retinal tear and retinal detachment risk.
Keywords
Coloboma
Optical coherence tomography
Stereoscopic vision
INTRODUCTION
Chorioretinal coloboma is a rare condition caused by incomplete closure of the embryonic fissure.[1] Typical colobomas occur in the inferior or inferonasal sectors of the retina, while atypical colobomas happen elsewhere.[2] Its prevalence is 0.14%, with an increased risk (up to 40%) of retinal detachment (RD) or neovascularization.[3] Advancements in multimodal imaging aid in understanding such cases. In this essay, we highlight the use of stereoscopic fundus photographs (SFPs), spectral-domain optical coherence tomography (SD-OCT), and fundus autofluorescence (FAF).
CASE REPORT
A 34-year-old woman underwent an eye examination without symptoms. Her best-corrected visual acuity was 20/20, and the slit-lamp examination revealed normal findings in both eyes. On fundus examination, a unilateral retinal and choroidal coloboma was observed in the right eye. SFP (CLARUS 500, Carl Zeiss Med Tech, Germany) highlighted its depth, extension, and location, 2.2 mm below the optic disc [Figure 1].
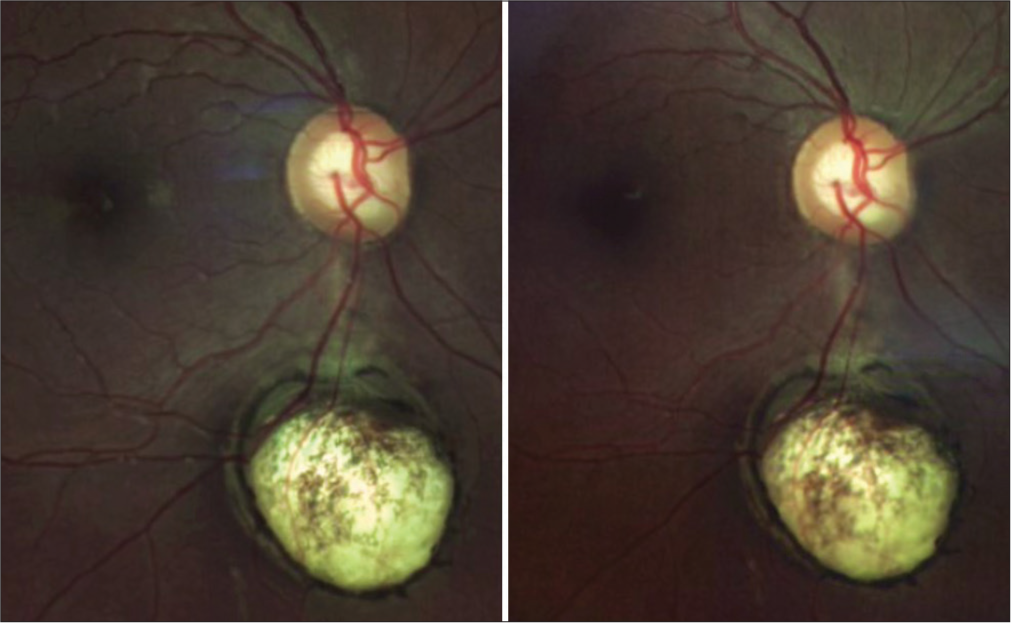
- Stereoscopic fundus photograph of the right eye. Chorioretinal coloboma and its depth, extension, and location are highlighted 2.2 mm below the optic disc.
On SD-OCT (CIRRUS 5000 HD, Carl Zeiss Med Tech, Germany), the coloboma was manually measured [Figure 2a, blue dashed line], showing 3,417 µm in width and 3,173 µm in height. At the deepest portion level, it measured 1,540 µm in length [Figure 2b, red dashed line]. Intercalary membrane (ICM) [Figure 2b, yellow arrowhead] associated with degenerative cavitations [Figure 2b, red asterisk] was observed without rupture of ICM, retinal tears or RD. In addition, the posterior hyaloid was detached above the coloboma area [Figure 2b, blue arrowhead].
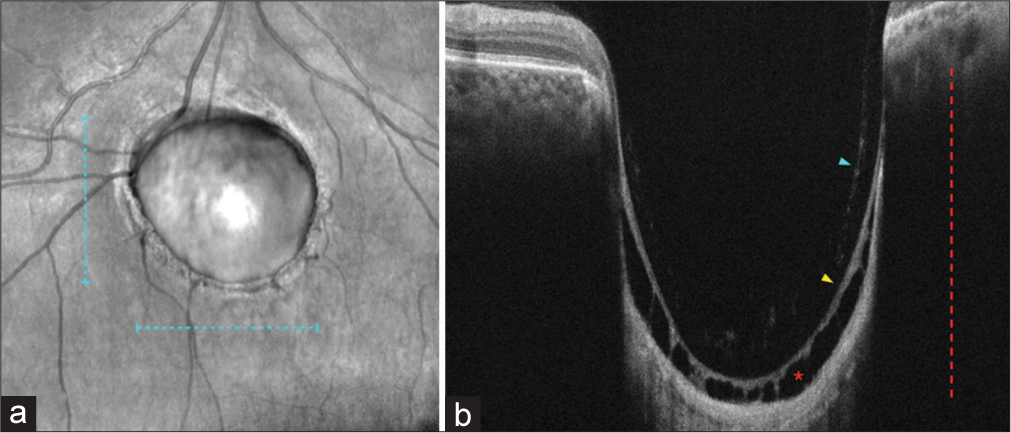
- (a) Infrared image shows coloboma dimensions: Width 3417 µm (blue dashed line) and height 3173 µm (blue dashed line). (b) Spectral-domain optical coherence tomography scan reveals coloboma length 1540 µm (red dashed line), posterior hyaloid (blue arrowhead), intercalary membrane (yellow arrowhead), and degenerative cavitations (red asterisk).
On FAF (CLARUS 500, Carl Zeiss Med Tech, Germany), a hyperautofluorescence line at the margin of the coloboma was observed [Figure 3a, red dashed line], corresponding to areas with partial absence of retinal layers in the OCT transition zone between the normal retina and the coloboma [Figure 3b, red dashed line]. In addition, hyporeflective foci with [Figure 3b, blue arrowhead] or without [Figure 3b, yellow arrowhead] shadows, corresponding to retinal vessels, were present.
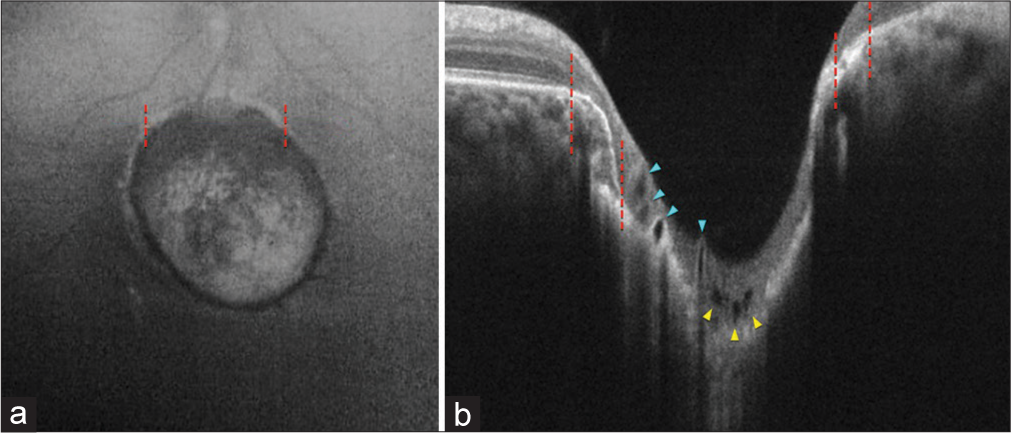
- (a) Fundus autofluorescence (FAF) reveals a hypoautofluorescence coloboma with a surrounding hyperfluorescent halo (red dashed lines). (b) Spectral-domain optical coherence tomography shows retinal atrophy with intact retinal pigment epithelium (red dashed lines), corresponding to the hyperfluorescent halo in FAF and hyporeflective foci with/without shadows (blue/yellow arrowheads), representing retinal vessels.
DISCUSSION
Retinochoroidal coloboma is a condition that is often stable or slow-growing.[1] Some cases present with poor vision, nystagmus, or white pupillary light reflex.[2] However, like ours, most patients are asymptomatic and diagnosed in a routine examination.
Recently, the neurosensory retina of the coloboma, known as the ICM, was described as particularly prone to rupture or RD.[4,5] Interestingly, retinal ruptures occurring outside the coloboma area have also been reported, suggesting additional abnormalities in the vitreoretinal interface.[2,4] Regular evaluations are essential for retinal tears or RD risk.
Prophylactic laser photocoagulation may be performed regarding the relatively high incidence of RD in such cases.[2,3] However, caution is needed near the macula, optic disc, or retinal nerve fiber layer (RNFL) close to the optic disc.[2] In our patient, we refrained from photocoagulation due to the proximity to the optic disc and the potential RNFL damage.
CONCLUSION
Multimodal imaging of chorioretinal colobomas can provide valuable information for diagnosing, monitoring, and managing this condition. In addition, regular eye examinations are crucial to detect changes in the coloboma or its surrounding tissues due to its related complications.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Uveal coloboma: Clinical and basic science update. Curr Opin Ophthalmol. 2006;17:447-70.
- [CrossRef] [PubMed] [Google Scholar]
- Ocular coloboma-a comprehensive review for the clinician. Eye (Lond). 2021;35:2086-109.
- [CrossRef] [PubMed] [Google Scholar]
- Chorioretinal coloboma complications: Retinal detachment and choroidal neovascular membrane. J Ophthalmic Vis Res. 2017;12:3-10.
- [CrossRef] [PubMed] [Google Scholar]
- Structural organization of choroidal colobomas of young and adult patients and mechanism of retinal detachment. Trans Am Ophthalmol Soc. 2005;103:457-72.
- [Google Scholar]







