Translate this page into:
The aqueous phase of neuroretinitis as a diagnostic challenge

*Corresponding author: Antonio López-Bolaños, Department of Retina and Vitreous, Instituto de Oftalmología Conde de Valenciana, Mexico City, Mexico. retina.lopez@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Illescas-Lomeli CA, Cortes-Muñoz D, RuizChavolla DE, López-Bolaños A. The aqueous phase of neuroretinitis as a diagnostic challenge. Lat Am J Ophthalmol. 2024;7:2. doi: 10.25259/LAJO_21_2023
Abstract
A 25-year-old man attended our office due to vision loss, metamorphopsia, headache, malaise, and fatigue. Visual acuity was 20/80 on the right eye and 20/20 on the left eye. On fundoscopy of the right eye, the optic nerve head (ONH) was elevated temporarily with the appearance of subretinal fluid from the ONH to the center of the macula. Since 1916, this entity has been studied, in the beginning, as “stellate maculopathy” by Theodor Leber until Donald Gass proved the origin of the fluid from the optic nerve vasculature, changing the nomenclature to neuroretinitis in 1977. The diagnosis of Neuroretinitis is challenging, specifically in the aqueous phase that can be confused by other macular entities. In this case, we present a patient with clinical and tomographic images in both aqueous and exudate phases with an interval of 3 weeks, intended to be representative of the pathological stages of neuroretinitis.
Keywords
Neuroretinitis
Pathological Phases
Stellate maculopathy
INTRODUCTION
Neuroretinitis is caused by an inflammation of the optic nerve head (ONH) and the neural retina. It presents with a classical clinical triad of vision loss, ONH edema, and macular exudates in the Henle’s layer with the typical star arrangement, usually unilateral.[1,2] Since 1916, this entity has been studied, in the beginning, as “stellate maculopathy” by Leber until Donald Gass proved the origin of the fluid leakage to come from the optic nerve vasculature, changing the pathology nomenclature to neuroretinitis in 1977.[3,4] The physiopathology is explained by direct invasion of infectious agents (predominantly bacteria and virus) or autoimmune response against the anterior portion of the optic nerve, ultimately with the inflammation of the ONH vasculature and consequent fluid leakage through the papillomacular bundle.[5] The clinical phases of Neuroretinitis can be described as follows: (a) Inflammation of the optic nerve and its vasculature, where edema of the ONH can be observed associated with elevation and telangiectasia of the superficial ONH vessels and (b) Aqueous phase: Increased vascular permeability of one or various vessels of the anterior optic nerve with variable degrees of fluid leakage, from the peripapillary region through the center of the macula. This leakage initially passes through the outer plexiform layer and the external limiting membrane, ultimately being able to collect in the subretinal space, causing a local neurosensory retinal detachment; (c) Exudative phase: It occurs days to weeks after first signs of visual impairment appear and is a result of the gradual edema resolution, leaving exudates within the Henle’s layer, giving the star-like disposition due to the radial arrangement of its fibers.[6] The cause of vision loss may be mainly due to intraretinal fluid (IRF) and subretinal fluid (SRF) rather than optic nerve dysfunction; this explains the favorable prognosis of this pathology and the little signs of optic nerve dysfunction.[7]
CASE REPORT
A 25-year-old man attended our office due to vision loss, metamorphopsia, and systemic symptoms such as headache, malaise, and fatigue. Visual acuity (VA) was 20/80 on the right eye and 20/20 on the left eye. No dyschromatopsia nor afferent pupillary defects were found. On pathological history, the patient was treated with antibiotic therapy for typhoid fever 1 year before the consultation. On fundoscopy of the right eye, the ONH was elevated temporarily with the appearance of SRF from the ONH to the center of the macula, with no pathological signs on fundoscopy of the left eye [Figure 1].

- A 25-year-old man fundoscopy. On the right eye, (a) the optic nerve head shows elevation on the temporal sector with the appearance of subretinal fluid to the center of the macula, (b) with no pathological signs in the left eye.
Optical coherence tomography (OCT) showed thickening of the layers of the retina with IRF and SRF, causing a local neurosensory retinal detachment and thickening of the ONH of the right eye [Figure 2]. Fluorescein angiography confirmed leakage from the optic nerve of the right eye [Figure 3].

- Optic coherence tomography showed thickening of the layers of the retina with intra-retinal and subretinal fluid, causing a local neurosensory retinal detachment and thickening of the optic nerve head of the right eye.
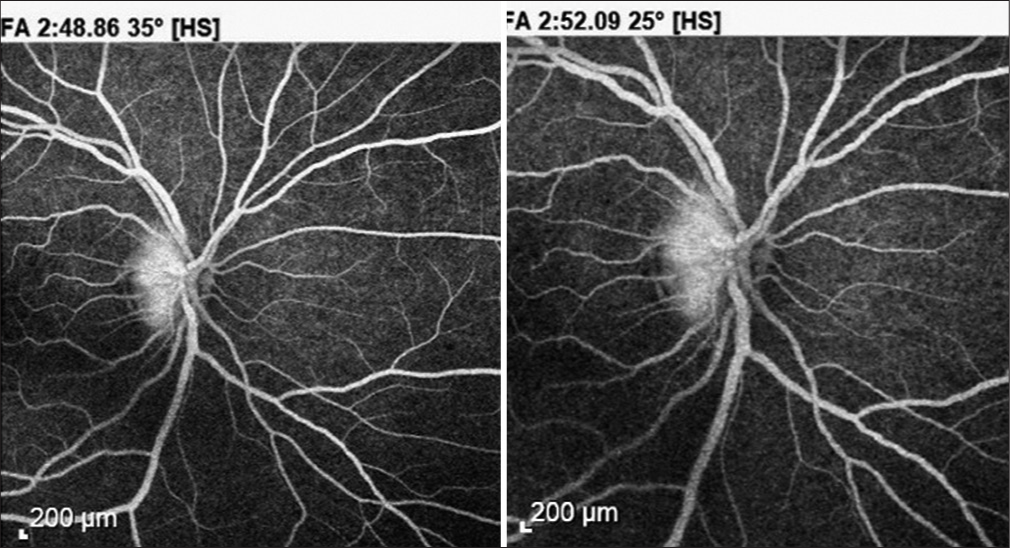
- Fluorescein angiography confirmed leakage from the optic nerve in late phases.
Even though therapeutic intervention with antibiotics and steroids lacks evidence, due to the moderate vision loss and the systemic symptoms and based on a review of evidence and expert opinion, antibiotic therapy was initiated with doxycycline 200 mg daily for six weeks. Three weeks after the beginning of the treatment, VA improved to 20/26 in the right eye, and systemic symptoms resolved; on fundoscopy of the right eye, the ONH edema and the apparent SRF were clinically resolved, with the consequent formation of the macular star by exudates [Figure 4]. OCT of the right eye demonstrated the resolution of the ONH edema, the SRF, and the new exudates deposited in the Henle’s layer [Figure 5].
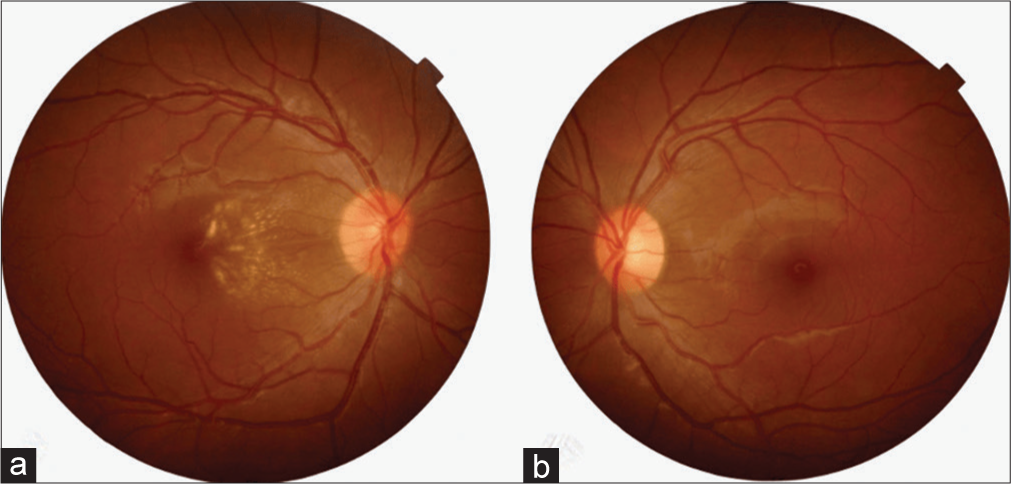
- Fundoscopy of the right eye (a) shows optic nerve edema and resolution of subretinal fluid, showing a macular star due to intraretinal exudates. (b) with no pathological signs in the left eye.
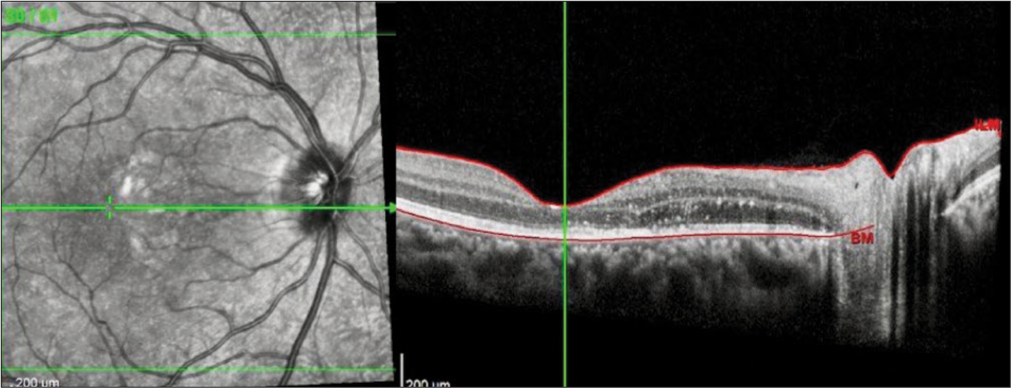
- Optical coherence tomography of the right eye demonstrates the resolution of the optic nerve head edema, the subretinal fluid, and the new exudates deposited in the Henle’s layer.
At week, the patient presented a complete improvement on VA (20/20); on fundoscopy examination and OCT imaging, exudates persisted but decreased in number and volume. Laboratory tests came negative for Tuberculin skin test, venereal disease research laboratory, human immunodeficiency virus, lyme serology, rocky mountain spotted fever testing, Typhoid and Bartonella serology, and general tests, including hematic biometry, were under normal range values. Therefore, the neuroretinitis was classified as idiopathic. The patient remains asymptomatic and under periodic surveillance.
DISCUSSION
Neuroretinitis is a challenging condition to diagnose, particularly during the aqueous phase. The clinical presentation of vision loss, ONH edema, and SRF is not specific to neuroretinitis and can overlap with other macular entities. In this case, the presence of SRF, clinical examination findings, and fluorescein angiography was crucial in confirming the diagnosis before the exudative phase, allowing for the initiation of appropriate treatment.[8]
The etiology of neuroretinitis can be related to direct invasion by infectious agents or an autoimmune response. In this case, the patient’s history of antibiotic therapy for typhoid fever suggests a possible infectious cause for neuroretinitis. However, laboratory tests for various infections returned negative, classifying the neuroretinitis as idiopathic.
Therapeutic intervention for neuroretinitis remains controversial, with limited evidence supporting the use of antibiotics.[9] In this case, antibiotic therapy with doxycycline was initiated, significantly improving VA and resolution of systemic symptoms. The favorable prognosis of neuroretinitis, characterized by minor optic nerve dysfunction was evident in the patient’s rapid recovery.
CONCLUSION
This case report highlights the challenges in diagnosing neuroretinitis during the aqueous phase and emphasizes the importance of a comprehensive diagnostic approach. Clinical history, thorough examination, and imaging modalities such as fluorescein angiography play a crucial role in achieving diagnostic certainty and initiating appropriate treatment. Despite the lack of definitive therapeutic guidelines, the favorable prognosis of neuroretinitis was demonstrated in this case, with significant visual improvement and resolution of symptoms.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Final diagnosis in patients referred with a diagnosis of neuroretinitis. Neuroophthalmology. 2015;39:266-70.
- [CrossRef] [PubMed] [Google Scholar]
- Die pseudonephritischen Netzhauterkrankungen, die Retinitisstellata; die purtschersche netzhautaffektion nach schwerer schädelverletzung In: Graefe AC, Saemisch T, eds. Graefe-Saemisch handbuch der gesamten augenheilkunde (2nd ed). Leipzig: Engelmann; 1916. p. :1319-39.
- [Google Scholar]
- Diseases of the optic nerve that may simulate macular disease. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83:763-70.
- [Google Scholar]
- Optic disk edema with a macular star. Surv Ophthalmol. 1998;43:270-4.
- [CrossRef] [PubMed] [Google Scholar]
- Neuroretinitis: Review of the literature and new observations. J Neuroophthalmol. 2011;31:58-68.
- [CrossRef] [PubMed] [Google Scholar]
- Neuroretinitis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570627 [Last accessed on 2023 Jun 19]
- [Google Scholar]
- Retinal angiography and optical coherence tomography disclose focal optic disc vascular leakage and lipid-rich fluid accumulation within the retina in a patient with leber idiopathic stellate neuroretinitis. J Neuroophthalmol. 2009;29:203-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective randomized double blind placebo-controlled evaluation of azithromycin for treatment of cat-scratch disease. Pediatr Infect Dis J. 1998;17:447-52.
- [CrossRef] [PubMed] [Google Scholar]







