Translate this page into:
Unilateral Purtscher’s retinopathy – A rare case report

*Corresponding author: Suraj Kumar Chaurasiya, Department of Optometry and Vision Science, CL Gupta Eye Institute, Moradabad, Uttar Pradesh, India. csurajk414@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chaurasiya SK, Lailung S, Agarwal P, Kohli P. Unilateral Purtscher’s retinopathy – A rare case report. Lat Am J Ophthalmol 2023:6:10.
Abstract
With retinal whitening (Purtscher’s flecken) and intraretinal hemorrhages, Purtscher’s retinopathy was initially reported as a symptom of sudden loss of vision following head trauma in 1910. A 28-year-old male patient presented with a history of sudden painless decrease of vision in his left eye (LE) for 1 week. He gave a history of head-and-neck injury following a road traffic accident. Unaided distance visual acuity was 20/20 in the right eye (RE) and 20/40 in the LE which improved up to 20/25 on pinhole at the time of presentation. On examination, the anterior segment was within normal limits. Fundus photo and ocular coherence tomography (OCT) showed normal in the RE; however, LE showed multiple white patches around the optic disc with flamed-shaped hemorrhages on the fundus photo and macular edema with discontinuity in the inner and outer retinal layer on OCT. The patient received oral steroids as treatment, and after 1 month of follow-up, had recovered to 20/20 visual acuity.
Keywords
Purtscher’s retinopathy
Head-and-neck injury
Road traffic accident
INTRODUCTION
Purtscher’s retinopathy is a rare sight-threatening condition associated with various types of trauma, which includes head trauma, seatbelt and airbag pressure, malar bone fracture, crush injury, and chest trauma.[1-4] Fundus examination revealed multiple areas of retinal whitening (Purtscher’s flecken) with intraretinal hemorrhages, sometimes accompanied by macular edema.[4] Here, we report a case of unilateral Purtscher’s retinopathy related to head-and-neck trauma after a road traffic accident.
CASE REPORT
A 28-year-old male patient presented to the retina clinic with a chief complaint of a sudden painless decrease of vision in his left eye (LE) for 1 week. He gave a history that he had been in a road traffic accident a week prior and had head-and-neck injuries, but without injury to the ocular or periorbital region. There was no history of diabetes or hypertension.
On external examination, head posture was normal with facial symmetrical on both sides; ocular motility was full in all directions. Unaided distance visual acuity was 20/20 in the right eye (RE) and 20/40 in the LE which improved up to 20/25 on pinhole at the time of presentation. On ocular examination, anterior segment examination was within normal limits, with normal pupillary reactions in both eyes. Intraocular pressure measured with Goldman Applanation tonometry was 15 mm of Hg in the RE and 16 mm of Hg in the LE, respectively. Fundus photo [Figure 1a] and ocular coherence tomography (OCT) showed normal in the RE [Figure 2a]; however, LE showed multiple white patches around the optic disc with flamed-shaped hemorrhages on the fundus photo [Figure 1b] and macular edema with discontinuity in the inner and outer retinal layer on OCT [Figure 2b]. The patient was managed with a short course of oral steroids. The oral steroid was given in a tapering dose for a period of 4 weeks. Over the course of 4 weeks, the unaided distance visual acuity improved from 20/40 to 20/20.
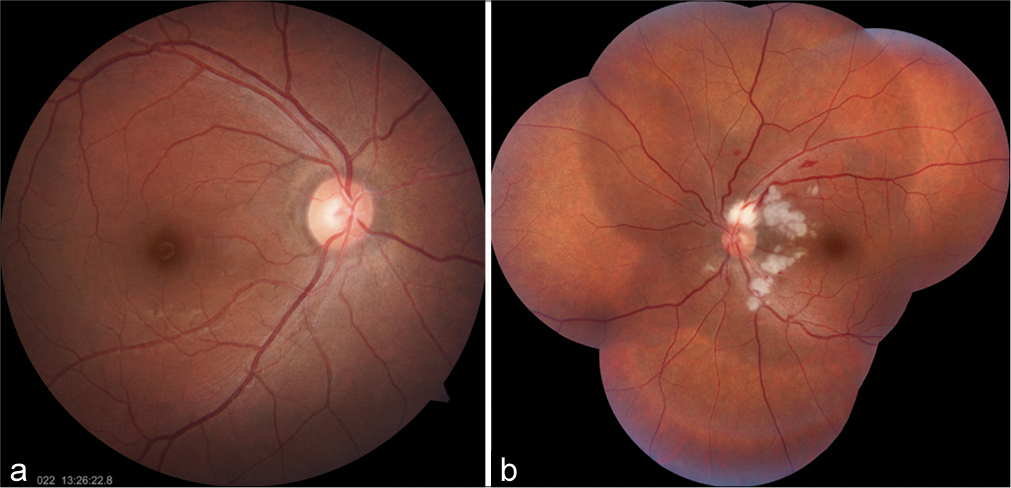
- (a) Right eye showing normal fundus photo. (b) Left eye showing multiple white patches around the optic disc with flamed-shaped hemorrhages.
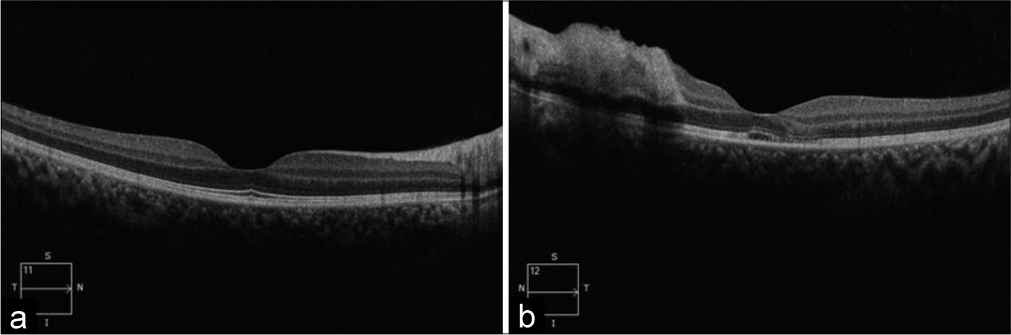
- (a) Ocular coherence tomography of the right eye shows normal. (b) Left eye showing macular edema with discontinuity in the inner and outer retinal layer.
DISCUSSION
Purtscher’s retinopathy (painful angiopathy of the retina that often follows head or chest injuries) should be considered a differential diagnosis in cases where visual loss is associated with multiple traumas. Dr. Otmar Purtscher first described Purtscher’s retinopathy in 1910 and also called “angiopathia retinae traumatica.”[4] Purtscher suffered from severe retinopathy following head trauma that was associated with vision loss.[4,5]
The pathophysiology of Purtscher’s retinopathy remains unclear. Previously, it was said that a sudden increase in intracranial pressure secondary to head injury led to retinal changes due to extravasation of lymph from retinal vessels.[6] Other causes are angiospasm from acute raised in intracranial or intrathoracic pressure, vascular emboli, and venous vasculitis caused by free fatty acids, air, fibrin, platelets, and leukocytes.[7] Leukoembolization, endothelial damage, activation of complement C5, and blockage of any small arterioles causing infarcts of the capillary bed have been implicated in the pathogenesis of Purtscher retinopathy. Leukoembolization is which is induced by the C5a complement. Complement C5a is associated with trauma, acute pancreatitis, and systemic vasculitic disease and has been proposed to play a role in the development of Purtscher’s retinopathy.[8] On the other hand, Purtscher’s like retinopathy can be associated acute pancreatitis, strenuous child birth, connective tissue disorders, and retrobulbar anesthesia.[9-11]
At present, there are no definite guidelines are set for the treatment of Purtscher’s retinopathy.[6] Wang et al.[12] reported a case of a patient who was given a mega-dose of steroid that showed an excellent visual response during the first 2 weeks of treatment. A patient, who had persistent a chest contusion, was treated with 39 courses of hyperbaric oxygen twice a week, which led to gradual improvement of visual function and retinal appearance.[13] We also treated our patient with oral steroids and he recovered to 20/20 in 4-week follow-up. Most patients usually improve without any treatment, with visual acuities generally improving to the 20/30–20/200 range. Visual prognosis is guarded, although initially, diminished vision may improve over a months.[14] There is no definite treatment for the disease but the role of corticosteroids is still debatable.
CONCLUSION
In conclusion, early corticosteroids treatment must be initiated to help these patients to restore their vision. Even though the patient will recover from their illness quickly with the usage of corticosteroids, the long-term negative effects of corticosteroid use, such as central serous retinopathy, weight gain, and avascular necrosis, also need to be taken into consideration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Purtscher retinopathy In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022.
- [Google Scholar]
- Systematic review of Purtscher's and Purtscher-like retinopathies. Eye (Lond). 2013;27:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of Purtscher's retinopathy treatments: A systematic review. Curr Eye Res. 2017;42:908-17.
- [CrossRef] [PubMed] [Google Scholar]
- Purtscher's retinopathy: Epidemiology, clinical features and outcome. Br J Ophthalmol. 2007;91:1456-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Purtscher's retinopathy: A case report. Del J Ophthalmol. 2016;27:30-2.
- [CrossRef] [Google Scholar]
- Purtscher's and Purtscher-like retinopathies: A review. Surv Ophthalmol. 2006;51:129-36.
- [CrossRef] [PubMed] [Google Scholar]
- Ballotini occlusion of retinal arteries. Collateral vessels. Br J Ophthalmol. 1966;50:482-95.
- [CrossRef] [PubMed] [Google Scholar]
- Purtscher-like retinopathy associated with acute pancreatitis. Sao Paulo Med J. 2005;123:289-91.
- [CrossRef] [PubMed] [Google Scholar]
- Purtscher's-like retinopathy after childbirth. Ophthalmology. 1990;97:1654-9.
- [CrossRef] [PubMed] [Google Scholar]
- Purtscher-like retinopathy after retrobulbar anesthesia. Ophthalmology. 1990;9:859-61.
- [CrossRef] [PubMed] [Google Scholar]
- Pathogenesis and neuroprotective treatment in Purtscher's retinopathy. Jap J Ophthalmol. 1998;42:318-22.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperbaric oxygen treatment in Purtscher's retinopathy induced by chest injury. J Chin Med Assoc. 2006;69:444-8.
- [CrossRef] [PubMed] [Google Scholar]






