Translate this page into:
Late-onset malignant glaucoma
*Corresponding author: Ramiro José Daud, MD, Deparment of Glaucoma, Instituto Altamira, Chubut, Argentina. ramiro.daud@institutoaltamira.com
-
Received: ,
Accepted: ,
How to cite this article: Daud RJ, Freile H, Freile M, Mariano S. Late- onset malignant glaucoma. Lat Am J Ophthalmol 2020;3:1.
Abstract
A case report on a 49-year-old female with diagnoses of ocular hypertension in her left eye (LE) treated with 250 mg/day acetazolamide for 2 years. During the slit-lamp examination, complete occlusion of both iridocorneal angles was detected. Intraocular pressure (IOP) was 10 and 35 mmHg in the right eye and LE, respectively. Phacotrabeculectomy was performed in the LE. After 1 month of the procedure, the patient developed a slowly progressive miopization from −1 to −3 diopters (D) the following months. Approximately 3 months after surgery, the patient developed an episode of acute pain, athalamia, and IOP 45 mmHg in her LE. Late-onset malignant glaucoma was suspected and the patient was treated with topical hypotensive and cycloplegic agent until a prompt vitrectomy was performed. Deepening of the anterior chamber and restoration of IOP to normal range was obtained after surgery.
Keywords
Glaucoma
Malignant glaucoma
Aqueous misdirection syndrome
Primary posterior capsulectomy
Irido-zonulo-hyaloido vitrectomy
INTRODUCTION
Malignant glaucoma is a recalcitrant and potentially devastating secondary angle-closure glaucoma. In 1869, Von Graefe described a rare post-operative complication characterized by flattening of the anterior chamber and elevated (intraocular pressure [IOP]). Diagnostic triad of a diffusely flat anterior chamber, IOP, and aqueous pooling that in sometimes is visible in or in front of the anterior vitreous is highly suggestive of malignant glaucoma. This can occur despite the existence of iridotomy or iridectomy. One hypothesis involves the misdirection of aqueous humor, or infused balanced salt solution at the time of cataract extraction, into or behind the vitreous body that is responsible for an increase vitreous volume and subsequent collapse of the anterior chamber. Another hypothesis involves choroidal expansion without actual misdirection of fluid.[1] The exact pathophysiologic mechanism of this disorder remains unclear. Malignant glaucoma has been reported following a wide variety of procedures including cataract extraction, trabeculectomy, phacotrabeculectomy, or implantation of several glaucoma devices. Although pars plana vitrectomy is an effective treatment for malignant glaucoma, is not always effective.[2]
CASE REPORT
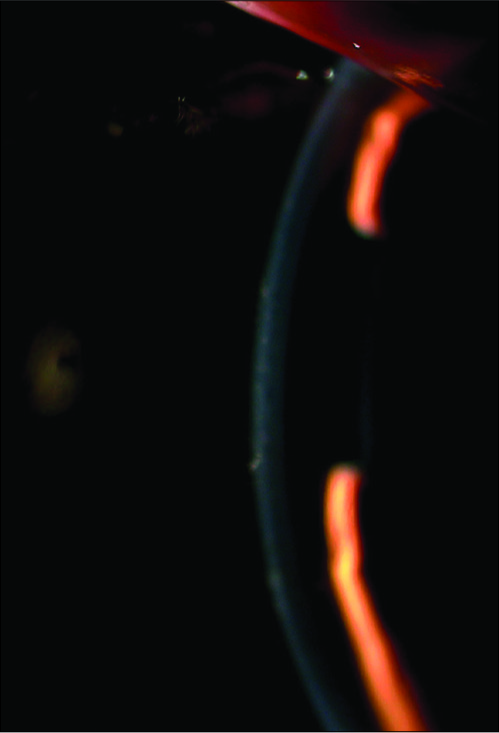
A 49-year-old with occluded iridocorneal angles in both eyes evaluated by gonioscopy despite a history of two peripheral iridotomies in both eyes presented with 35 mmHg IOP that did not respond to medical therapy. Better-corrected visual acuity was 20/20 (+1.50) in the right eye and 20/20 (+2.50) in the left eye (LE). Slit-lamp examination revealed narrow anterior chamber both eyes. A pronounced optic disk excavation was in accordance with pathologic campimetry in the LE [Figure 2]; phacotrabeculectomy in the LE was performed. One week after the procedure, the patient presented spherical equivalent (SE) of −1 and IOP of 12 mmHg. One month after surgery, a SE of −3 in the LE was recorded and IOP of 15 mmHg. Approximately 3 months after surgery, the patient suddenly present acute pain, athalamia [Figure 4], and IOP of 45 mmHg in her LE. The event was interpreted as malignant glaucoma, and therefore, treatment with topical hypotensive and cycloplegic agents was initiated until an emergency vitrectomy was performed [Figure 5].
- Slit-lamp examination revealed narrow anterior chamber both eyes.

- Visual field testing.
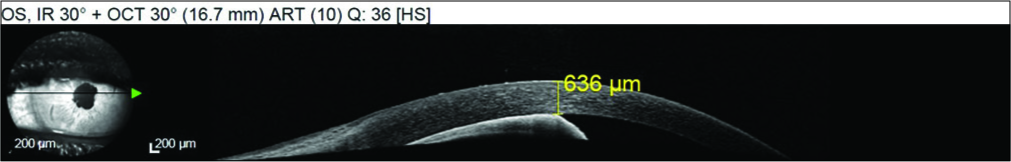
- SD-OCT performed on the day of malignant glaucoma where atalamia, iridoendotelial contact, and increased corneal thickness are observed.

- 24 hours post-vitrectomy anterior chamber.
DISCUSSION
While malignant glaucoma is an acute process characterized by pain, ocular hypertension and flattening of the anterior chamber is an entity that is generally described as an immediate post-operative event with a reserved visual prognosis. In the case report, the patient presented with progressive myopization with normal IOP and the classic triad of malignant glaucoma developed 3 months post- operative. Vitrectomy was performed to create a unique chamber that restores the fluid mechanics of aqueous humor. We did not find any case in the current bibliography that presents the events of our patient. The cases described were presented with the classic triad from months to years after a surgical procedure.
We find this case relevant for the ophthalmic literature given it illustrates that malignant glaucoma can present even months after surgery and an accurate diagnosis must be reached promptly to act accordingly to prevent irreversible consequences.[3-5]
CONCLUSION
While acute glaucoma must be treated early and aggressively to preserve the best possible visual function, the prognosis remains poor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Fluid misdirection syndrome: The unified definition of malignant glaucoma. J Glaucoma. 2019;28:e165.
- [CrossRef] [PubMed] [Google Scholar]
- Acute and chronic fluid misdirection syndrome: Pathophysiology and treatment. Graefes Arch Clin Exp Ophthalmol. 2018;256:135-54.
- [CrossRef] [PubMed] [Google Scholar]
- Management of recurrent aqueous misdirection by anterior segment surgeon after failed pars plana posterior vitrectomy. Indian J Ophthalmol. 2019;67:1204-6.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic fluid misdirection syndrome of aqueous humor after phacoemulsification: Diagnosis, treatment and asscociated factors. Arch Soc Esp Oftalmol. 2019;94:491-4.
- [CrossRef] [PubMed] [Google Scholar]
- Intra-operative ostial irido-zonulo-hyaloido-vitrectomy with primary posterior capsulectomy for prevention of post-operative aqueous misdirection in combined phaco-trabeculectomy in primary angle closure glaucoma. Curr Eye Res. 2019;44:1087-90.
- [CrossRef] [PubMed] [Google Scholar]






