Translate this page into:
Eyeing risks: Navigating ophthalmic challenges in sinus surgery

*Corresponding author: Amber Dubey, Department of Vitreo Retina, Sri Sankaradeva Nethralaya, Guwahati, Assam, India. dubeyamber25@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Dubey A, Venkatraman V, Barman M, Bhattacharjee K. Eyeing risks: Navigating ophthalmic challenges in sinus surgery. Lat Am J Ophthalmol. 2023;6:19. doi: 10.25259/LAJO_22_2023
Abstract
This is a descriptive case report of a 25-year-old male who presented with right eye diminution of vision associated with ophthalmoplegia and strabismus following functional endoscopic sinus surgery (FESS) for deviated nasal septum. On examination, he had a large angle right exotropia with enophthalmos and restricted extra ocular movements. Pupils were dilated and fixed suggestive of optic neuropathy and fundus revealed a central retinal artery occlusion. Multimodal radiological imaging revealed optic nerve sheath hematoma, fracture of medial orbital wall and orbital floor along with medial rectus disinsertion with posterior discontinuation. Due to delayed presentation at our clinic, he was managed conservatively with intravenous and oral corticosteroids. The patient displayed mild improvement in ocular movement and vision. He was advised orbital reconstruction of the medial wall and floor for enophthalmos correction and cosmesis. Although a relatively safe procedure, FESS can result into varied orbital complications, including damage to the extraocular muscles, optic nerve and its vascular supply. This case report, to the best of our knowledge is the first of its kind to document ophthalmoplegia due to medial rectus disinsertion along with central retinal artery occlusion. It also highlights the perioperative risk factors and provides insight into the intraoperative signs to be cautious of during sinus surgeries
Keywords
Functional endoscopic sinus surgery
Optic nerve sheath hematoma
Paralytic strabismus
Orbital floor fracture
Enophthalmos
Central retinal artery occlusion
INTRODUCTION
Functional endoscopic sinus surgery (FESS) is a relatively safe procedure indicated for deviated nasal septum, and chronic rhinosinusitis with an expanding role in the management of other sinus, orbit, and skull base diseases.[1] The proximity of the sinus with orbits and congenital variations in the anatomy of the medial wall, with inherent deficiency of lamina papyracea, prove to be a risk factor for ophthalmic mishaps. An ophthalmologist’s perspective on understanding ominous signs can help earlier identification and prevention of these catastrophic complications.
In this case report, we highlight the perioperative risk factors and insight into the ominous intraoperative signs during sinus surgeries.
CASE REPORT
A 25-year-old young man presented to our clinic with complaints of the right eye diminution of vision associated with deviation of eyes following surgery for a deviated nasal septum. As per records, he had undergone FESS 1 week back. On examination, the right eye pupils were dilated and fixed with best-corrected visual acuity of counting fingers (CF) 3 m. On external examination, the eye was deviated laterally with restriction of extra ocular movements in all gazes [Figure 1]. Modified Krimsky test showed right exotropia of 95 prism diopter (Base IN). Hertel’s exophthalmometry showed enophthalmos (OD– 13 mm OS–18 mm Base–95 mm) with a deep superior sulcus. The anterior segment was unremarkable, while the fundus showed diffuse retinal whitening suggestive of Central Retinal Artery occlusion (CRAO). Optical coherence tomography showed inner/middle retinal hyperreflectivity suggestive of inner retinal edema. Fundus fluorescein angiography revealed delayed transits (16 s) with irregular foveal hypofluorescence due to inner retinal edema in the macular region [Figures 2a-2c]. Visual fields (HVF 30–2) showed severe depression of the field with a visual field index <1%, and visual-evoked potential showed diminished waveforms with decreased amplitudes.

- External photograph in the primary and secondary gaze showing right eye deviated laterally and enophthalmos with restriction of extraocular movements in all gazes.
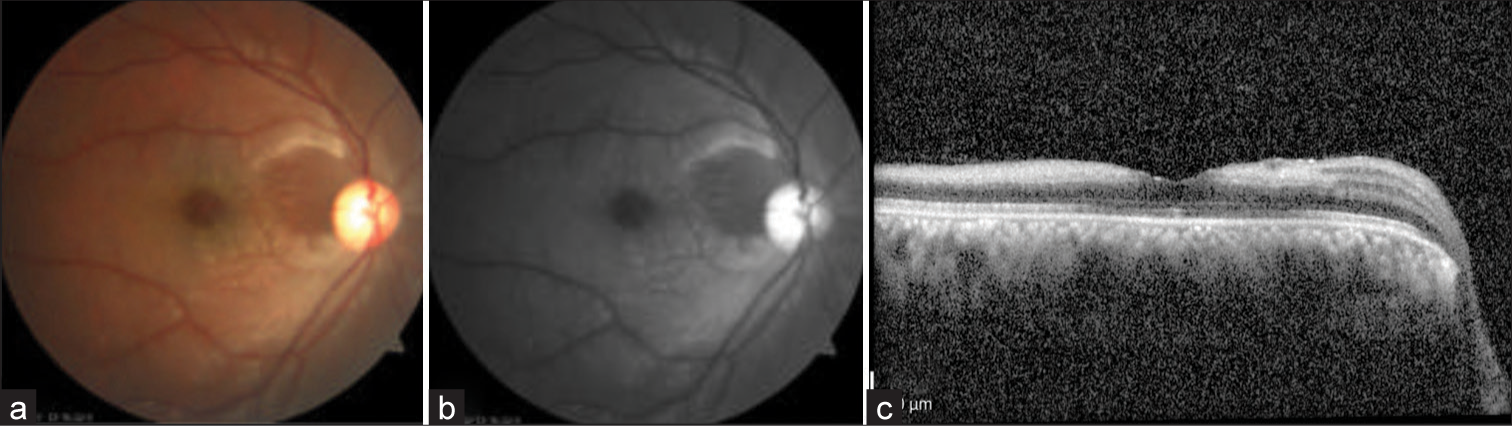
- (a) Fundus photograph showing diffuse retinal whitening, (b) fundus fluorescein angiography showing irregular foveal hypo fluorescence, and (c) optical coherence tomography showing inner/middle retinal hyperreflectivity.
Computed tomography (CT) scan was suggestive of an area of dehiscence in the right lamina papyracea with focal inconspicuous medial rectus muscle associated with a fracture of the orbital floor on the right side with displacement of bone fragment into the maxillary antrum. A small hematoma was noted in the right periorbital space in the anterosuperior aspect in the extraconal space extending posteriorly along the superior orbital roof, diminishing posteriorly, measuring 16 × 5 mm (trans × thickness) without intraconal extension. The immediate retrobulbar right optic nerve was thickened (5.4 mm) with kinking and ill-defined margins and diffuse low-signal intensity of optic nerve sheath complex with loss of perineural cerebrospinal fluid space suggestive of optic nerve sheath hemorrhage causing compression. Contrast-enhanced magnetic resonance imaging ORBIT showed discontinuity of the right medial rectus muscle [Figures 3a and 3b].
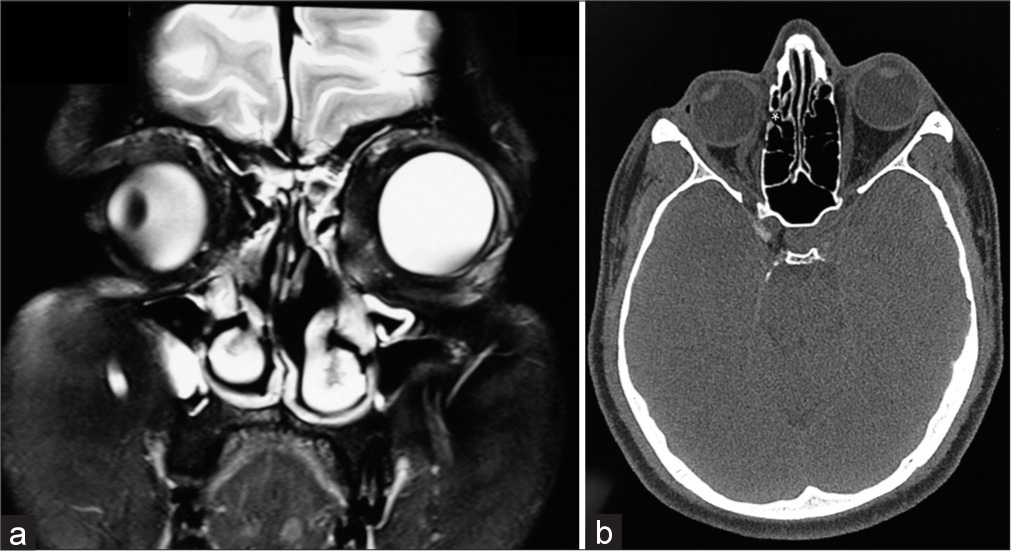
- (a) T2-weighted fat-suppressed coronal magnetic resonance imaging of the orbits showing laterally rotated right globe with distortion of the medial wall of the right orbit post endoscopic sinus surgery. (b) Non-contrast axial computed tomography image of the orbits highlights the disinsertion of the medial rectus from the site of insertion on the right globe.
The patient was initially managed with intravenous methylprednisolone 1 g/day for three days, along with weekly tapering oral corticosteroids (1 mg/kg/body weight),with mild improvement in ocular movements and vision. The associated central artery occlusion led to significant visual morbidity. Surgical exploration with repair for cosmetic correction was advised; however, the patient was unwilling for any further surgical intervention.
DISCUSSION
Ophthalmic complications of FESS are rare, with a reported incidence of 0.5–5%.[1,2] These include ecchymosis, medial wall fracture, emphysema, retro-orbital hemorrhage, lacrimal duct injury, optic neuropathy, muscle injury, and CRAO.[2]
Pre-operative imaging can help detect anatomical variations, namely, inherent deficiency of the medial wall, and surgical approach planned accordingly. Documentation of any predisposing conditions or pre-operative visual deficits, as well as informed consent, is essential.[2]
Intraoperative pupillary examination is prudent in all surgeries involving orbital manipulation to circumvent any iatrogenic damage. To facilitate such an examination during the surgery, pre-operative dilating topical medication or contact with ocular anesthetic agents containing epinephrine must be avoided. Affirmation of direct optic nerve injury can be assessed only by eliciting a new relative afferent pupillary defect and not a mere pupillary dilatation. Pupillary peaking or distortion in pupillary anatomy might be indicative of injury to the parasympathetic pupillomotor ciliary ganglion.[3]
Optic nerve sheath hematoma should be managed with a combination of surgery and corticosteroids on a case-dependent approach. Wu et al. advised treatment with methylprednisolone if a patient presents within 8 h of insult and optic canal decompression within 12–24 h of beginning medical treatment.[4,5]
The ominous perioperative signs of retrobulbar hemorrhage that should raise suspicion of raised intraorbital pressure secondary to retro-orbital hemorrhage include sudden onset and progressive proptosis, pain, chemosis, and ophthalmoplegia. It is prudent to leave the eye open and pupillary reflexes frequently assessed for early detection and decompression if indicated to prevent optic neuropathy secondary to direct compression. In such a scenario, lateral canthotomy can help relieve pressure and prevent further complications.[2,6]
CRAO post-sinus surgery is sequential to vascular occlusion as a result of orbital compartment syndrome. An orbital decompression within 90 min of suspected diagnosis is crucial to preclude permanent optic nerve damage. Kurt et al. highlighted that one must consider comorbidities such as diabetes mellitus and coronary artery disease, wherein perfusion impairment can predispose the patient to orbital hemorrhage.[7] Parikh et al. have reported that proximal optic nerve diffusion restriction in brain MRI can be diagnostic of proximal thromboembolic CRAO.[8]
Our patient had extraocular excursion limitation with large angle right exotropia secondary to medial rectus disinsertion along with sixth nerve palsy. The incidence of paralytic strabismus following FESS is relatively low. The most common cause for paralytic strabismus is direct muscle injury, with the medial rectus being the most common muscle involved due to its proximity to lamina papyracea.[2]
The major limitation in our case was the delayed presentation of the patient at our clinic. Early detection is primary to the treatment of CRAO. Retinal infarction occurs within 90– 240 min of CRAO, with ganglion cell death occurring within 12–15 min.[9] A general treatment guideline does not exist for CRAO; however, it can combated with various modalities such as pentoxifylline, inhalation of carbogen, sublingual isosorbide dinitrate, ocular massage with three mirror contact lens, acetazolamide, mannitol, methylprednisolone, tissue plasminogen activator, surgical modalities such as anterior chamber paracentesis, Neodymium: Yttrium-aluminiumgarnet laser, and pars plana vitrectomy with removal of the embolus among others, in different combinations with reported visual recovery with the early treatment and presence of cilioretinal artery.[10]
CONCLUSION
We establish that a more holistic understanding and multidisciplinary approach to such cases can avert untoward incidences. This case report, to the best of our knowledge, is the first of its kind to document ophthalmoplegia due to medial rectus disinsertion along with CRAO. Early detection and management by an ophthalmologist are key to improving prognosis and patient outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Ophthalmic complications of endoscopic sinus surgery. Surv Ophthalmol. 2003;48:389-402.
- [CrossRef] [PubMed] [Google Scholar]
- Ophthalmic complications of endoscopic sinus surgery. Braz J Otorhinolaryngol. 2017;83:318-23.
- [CrossRef] [PubMed] [Google Scholar]
- Principles of protection of the eye and vision in orbital surgery. J Neurol Surg B Skull Base. 2020;81:381-4.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic optic nerve sheath hematoma. Case Rep Ophthalmol. 2021;12:569-73.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic optic neuropathy therapy: An update of clinical and experimental studies. J Int Med Res. 2008;36:883-9.
- [CrossRef] [PubMed] [Google Scholar]
- Review of management options for a retrobulbar hemorrhage. J Oral Maxillofac Surg. 2007;65:296-9.
- [CrossRef] [PubMed] [Google Scholar]
- A rare complication of endoscopic sinus surgery: Retinal artery occlusion. Eur J Ophthalmol. 2019;29:NP9-11.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral optic nerve diffusion restriction after sinus surgery secondary to central retinal artery occlusion: Case report and literature review. Neurologist. 2023;28:46-8.
- [CrossRef] [PubMed] [Google Scholar]
- Central retinal artery occlusion-rethinking retinal survival time. BMC Ophthalmol. 2018;18:101.
- [CrossRef] [PubMed] [Google Scholar]
- Central retinal artery occlusion after nasosinal surgery-an insight. Int Med Case Rep J. 2020;13:211-5.
- [CrossRef] [PubMed] [Google Scholar]







