Translate this page into:
Multiple evanescent white dot syndrome following COVID-19 infection: A case report

*Corresponding author: Sara Hemmati, Department of Ophthalmology, Iran University of Medical Sciences, Tehran, Iran. hemmati1373@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Abdi F, Hemmati S, Sharafinejad M, Gordiz A, Aghili S, Zare Hosseinabadi V. Multiple evanescent white dot syndrome following COVID-19 infection: A case report. Lat Am J Ophthalmol. 2023;6:18. doi: 10.25259/LAJO_13_2023
Abstract
Multiple evanescent white dot syndrome (MEWDS) is typically a unilateral and transient condition without an exact known underlying cause. Its pathogenesis may involve an immune response to viral antigens that have gained access to the retinal receptor cells. It has been hypothesized that the COVID-19 virus can activate some autoimmune responses. Here, we report a case of MEWDS in a 16-year-old girl with a history of COVID-19 infection two weeks before the visual symptoms. The symptoms and signs improved without any treatment after a three-month follow-up period. In our case, MEWDS occurred shortly after COVID-19 infection and resolved without treatment in three months. Considering ophthalmologic and immunologic associations of COVID-19 can help ophthalmologists in the diagnosis and treatment of similar disorders in the COVID-19 era.
Keywords
Multiple evanescent white dot syndrome
COVID-19
Coronavirus
INTRODUCTION
The World Health Organization declared that coronavirus 2019 infection (COVID-19) has led to a pandemic in March 2020.[1] COVID-19 is a complex disease which can affect many parts of the human body.[2] Ophthalmologic symptoms and signs are reported to be the presenting and even only manifestations of this disorder.[3]
Multiple evanescent white dot syndrome (MEWDS) is typically a unilateral syndrome which usually occurs acutely and manifests with transient small dots at the level of the outer retina and retinal pigment epithelium and foveal granularity. Other signs may include optic nerve head edema, mild anterior chamber reaction, and vitritis.[4] In about one-third of patients, a viral illness occurs before the onset of the disease.[5]
The underlying pathogenesis of MEWDS is not exactly clear, but it may involve an immune response to viral antigens that have gained access to the retinal receptor cells.[4,5] It has been hypothesized that the COVID-19 virus can activate some autoimmune responses.[6]
Here, we report a case of MEWDS that occurred following COVID-19 infection.
CASE REPORT
A 16-year-old girl came to our clinic with a chief complaint of blurred vision in her left eye. Her past medical history included a COVID-19 infection two weeks before the onset of her visual symptoms. No other medical history or family history was mentioned. On examination, the best corrected visual acuity (BCVA) was ten out of ten in her right eye and five out of ten in her left eye. There was no afferent pupillary defect, and intraocular pressure was within normal limits in both eyes. In the anterior segment examination, no pathological finding was detected, and there was no anterior chamber reaction in either eye. As shown in Figure 1a-c, fundus photograph [Figure 1a], fundus autofluorescence (FAF) [Figure 1b] and macular optical coherence tomography (OCT) [Figure 1c] of the right eye is normal at the time of presentation. On the other side, fundoscopic examination of the left eye revealed diffuse, subtle, deep, yellow lesions in the retina with a typical foveal granularity [Figure 1d]. Moreover, fundus autofluorescence (FAF) revealed multiple hyperautofluorescent patches throughout the macula and mid-peripheral retina [Figure 1e] and Optical coherence tomography (OCT) demonstrated attenuation of the ellipsoid and interdigitation zones in the left eye [Figure 1f]. Based on these findings, the patient was diagnosed with MEWDS, and follow-up was recommended. According to Figure 2a-c, fundus photograph [Figure 2a], FAF [Figure 2b] and macular optical coherence tomography (OCT) [Figure 2c] of the right eye is normal at the three-month follow-up. The patient also reported improved vision in her left eye and BCVA improved to 10 out of 10 after the same duration of time. Fundus examination showed a decrease in the prominence and number of the deep retinal yellow lesions during three months [Figure 2d]. Besides, FAF showed fading of the hyper-fluorescence patches at this point [Figure 2e] and OCT demonstrated reconstitution of the ellipsoid zone [Figure 2f].
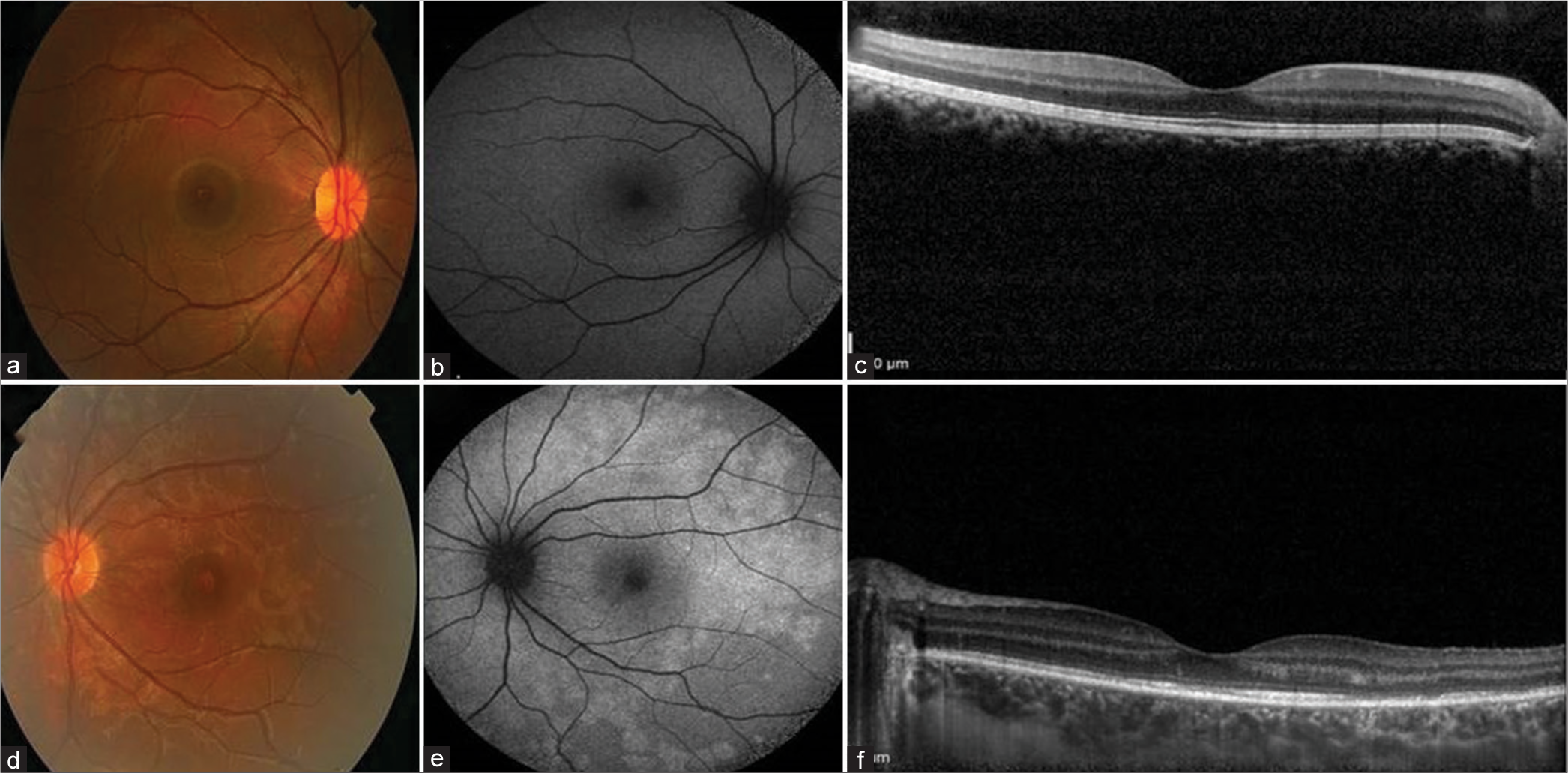
- Imaging of both eyes at the time of presentation. (a) Fundus photograph, (b) fundus autofluorescence (FAF), and (c) macular optical coherence tomography (OCT) of the right eye is normal. (d) Fundus photograph of the left eye shows subtle deep, yellow lesions in the retina and foveal granularity. (e) FAF of the left eye demonstrates a ring of circumpapillary hyperautofluorescence and surrounding scattered small foci of hyperautofluorescence. (f) OCT of the left eye hows attenuation of the ellipsoid and interdigitatsion zones.
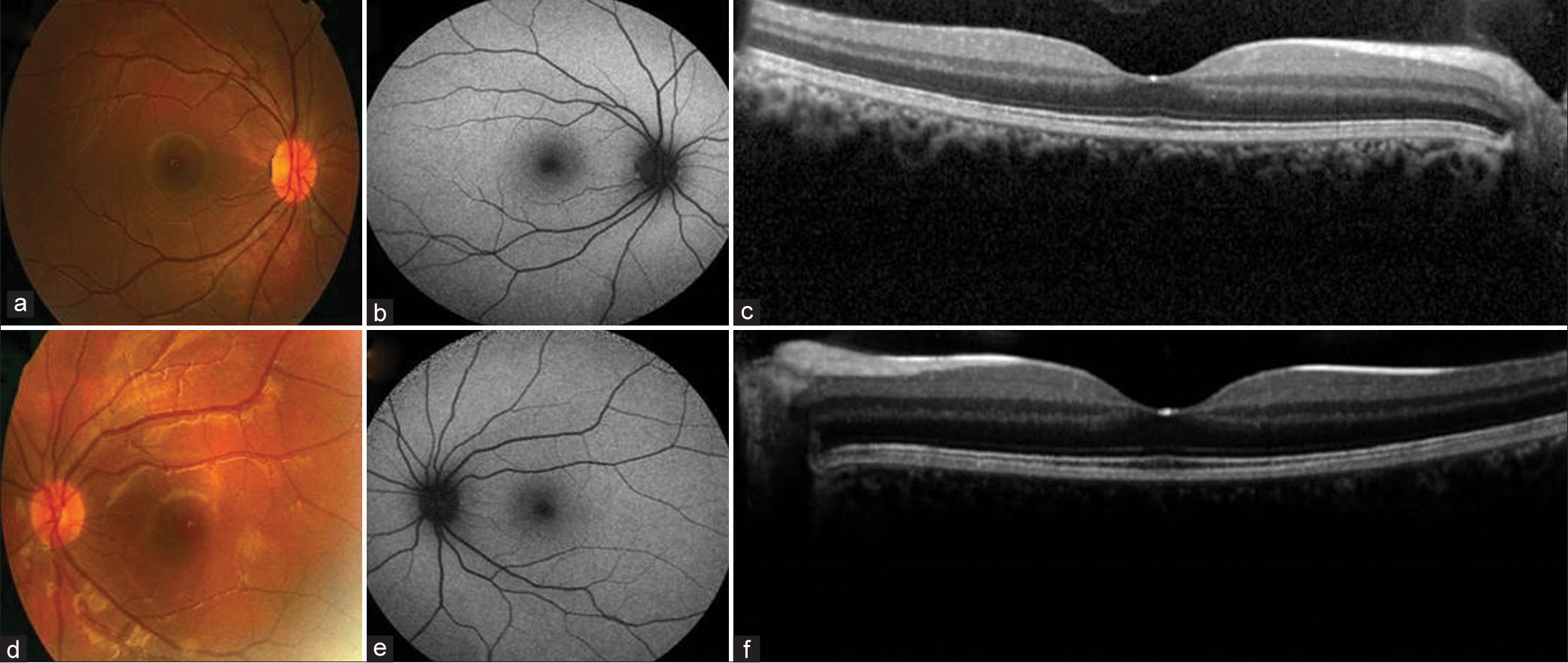
- Imaging of both eyes at the three-month follow-up.(a) Fundus photograph, (b) fundus autofluorescence (FAF), and (c) macular optical coherence tomography (OCT) of the right eye is normal. (d) In the fundus photograph of the left eye, there is a decrease in the number and prominence of the deep retinal yellow lesions. (e) FAF of the left eye is nearly normal. (f) Macular OCT of the left eye shows reconstitution and recovery of the ellipsoid zone.
DISCUSSION
MEWDS is an idiopathic disorder without an exact known pathogenesis.[7] An immune response to viral antigens that have gained access to the retinal receptor cells could have a role in the pathogenesis of this disorder.[7] It is hypothesized that the COVID-19 virus can activate some autoimmune responses.[6] Suggestive clues include the increased prevalence of autoantibodies in patients with this infection and also the susceptibility of patients with autoimmune disorders to COVID-19 infection.[6] It has also been proposed that a phase of autoimmunity can occur following COVID-19 infection.[7]
A few cases of MEWDS following COVID-19 infection are reported in the literature. Jain et al. reported a 17-year-old boy with MEWDS about two months after SARS-CoV-2 infection, which responded well to oral corticosteroids.[7] There is also a case report describing an atypical case of MEWDS following COVID-19 infection in which there was no classic hypocyanescent lesion in indocyanine green angiography (ICGA), and instead, multiple hypercyanescent lesions were noted.[8] Furthermore, Conrady et al. reported a case with acute outer retinopathy similar to MEWDS but without complete recovery of vision.[9]
On the other hand, Azar et al. reported that although MEWDS is possibly associated with inflammation and immunity, the incidence of MEWDS did not show a rise during the COVID-19 pandemic in their center.[10]
CONCLUSION
In our case, MEWDS occurred shortly after COVID-19 infection and resolved without treatment in three months. Considering ophthalmologic and immunologic associations of COVID-19 can help ophthalmologists in the diagnosis and treatment of similar disorders in the COVID-19 era.
Ethical approval
The study was approved by the Institutional Ethical Committee at Iran University of Medical Sciences as a case report.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- COVID-19: A complex multisystem disorder. Br J Anaesth. 2020;125:238-42.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 and eye: A review of ophthalmic manifestations of COVID-19. Indian J Ophthalmol. 2021;69:488-509.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple evanescent white dot syndrome (MEWDS) Int Ophthalmol Clin. 2012;52:221-8.
- [CrossRef] [PubMed] [Google Scholar]
- Serpiginous choroiditis presenting after SARS-CoV-2 infection: A new immunological trigger? Eur J Ophthalmol. 2022;32:NP97-101.
- [CrossRef] [PubMed] [Google Scholar]
- Multiple evanescent white dot syndrome following SARS-CoV-2 infection-a case report. Indian J Ophthalmol. 2022;70:1418-20.
- [CrossRef] [PubMed] [Google Scholar]
- An uncommon cold of the retina. Surv Ophthalmol. 2022;67:1553-8.
- [CrossRef] [PubMed] [Google Scholar]
- Coronavirus-19-associated retinopathy. Ocul Immunol Inflamm. 2021;29:675-6.
- [CrossRef] [PubMed] [Google Scholar]
- Did the COVID-19 pandemic increase the incidence of acute macular neuroretinopathy? J Clin Med. 2021;10:5038.
- [CrossRef] [PubMed] [Google Scholar]






