Translate this page into:
Systematic review of surgical techniques for treating giant retinal tears in adults: A current assessment of approaches and interventions

*Corresponding author: Miguel Angel Quiroz-Reyes, Department of Retina, Oftalmologia Integral ABC, Mexico City, Mexico. drquiroz@prodigy.net.mx
-
Received: ,
Accepted: ,
How to cite this article: Quiroz-Reyes MA, Quiroz-Gonzalez EA, Quiroz-Gonzalez MA, Lima-Gomez V. Systematic review of surgical techniques for treating giant retinal tears in adults: A current assessment of approaches and interventions. Lat Am J Ophthalmol. 2024;7:12. doi: 10.25259/LAJO_15_2024
Abstract
Giant retinal tears (GRTs) are rare and challenging complications of rhegmatogenous retinal detachment (RRD) that necessitate intricate surgical management. This study aimed to systematically review and analyze the functional outcomes, anatomical success rates, and complications associated with surgical interventions for GRTs in adults. A comprehensive literature search was conducted using electronic databases, including PubMed, Embase, Web of Science, and the Cochrane Library, from 2002 to February 2024. We included original research articles with diverse study designs involving adult patients (≥18 years) who underwent surgical treatment for GRTs. The identified interventions included pars plana vitrectomy, scleral buckling, combined procedures, and pneumatic retinopexy. The outcome measures included detailed descriptions of pre-and post-operative visual acuity, initial and final anatomical success rates, and main post-operative complication descriptions. After screening 4104 records, 22 studies were ultimately included in the study. The total sample comprised 1607 participants, with a male predominance. Surgical interventions have resulted in varying improvements in post-operative visual acuity. Notably, the anatomical success rates ranged from 70% to 100%, with microincision vitrectomy surgery (MIVS) platforms currently being the predominant gold-standard surgical method for GRT-associated RRDs. The postoperative complications identified were proliferative vitreoretinopathy (PVR), epiretinal membrane (ERM) development, hypotony, cataracts, uveitis, and foreign body reaction. Subsequent examination revealed poor pre-operative visual acuity, pre-operative PVR, and younger age, which presented challenges that impacted the outcomes. Despite limited evidence, this systematic review offers valuable insights into the diverse outcomes and difficulties associated with surgical approaches and interventions for GRTs in the adult population. This study highlights the significance of management strategies and calls for additional research in this field.
Keywords
Giant retinal tears
Rhegmatogenous retinal detachment
Microincision vitrectomy surgery
Proliferative vitreoretinopathy
Scleral buckling
Macular pucker
Short-term post-operative tamponade
INTRODUCTION
A giant retinal tear (GRT) is a full-thickness retinal break that extends 90° or more circumferentially in the presence of posterior vitreous detachment.[1,2] Approximately 1% of rhegmatogenous retinal detachments (RRDs) are associated with GRT, with an estimated incidence of 0.1 cases/100,000 people per year in the general population.[2-4] Its incidence is usually greater in males (72%) than in females.[2] The majority of GRTs have no identifiable cause (idiopathic),[5] although they can be linked to different factors, such as high myopia, trauma, Ehlers-Danlos syndrome, Marfan syndrome, and hereditary vitreoretinopathies, including Stickler syndrome.[2,6,7] Moreover, wide areas of lattice degeneration and white without pressure lesions are considered potential risk factors.[2]
Adult GRTs exhibit changes in their central or core vitreous gel, leading to syneresis and liquefaction. These changes resulted in the formation of large, central lacunae. As the condition progresses, the peripheral gel condenses, and its posterior aspect forms a transvitreal membrane oriented along the equator. Contraction of this membrane causes retinal tearing at the posterior border of the vitreous base. However, vitreous syneresis and liquefaction are not observed in children. This absence is attributed to the presence of type IX collagen, which coats the outer surface of type II collagen within the vitreous. This coating prevents collagen fibrils from adhering to each other and may also account for the robust adherence of the vitreoretinal interface.[8] In contrast, hereditary vitreoretinopathies and pathological myopia exhibit vitreous liquefaction and fibrillar collagen condensation, indicating the occurrence of GRTs at a younger age.[8] Although Weinberg et al. reported that the incidence of pediatric RRD due to GRT was 5.6%, a few studies have reported a higher incidence of GRT-associated RRD (15– 20%).[9,10] However, in adults, the reported incidence of GRT-associated RRD is lower (0.5–8.3%).[11,12]
Due to the extent of exposure of the retinal pigment epithelium (RPE) the rapid development of pre-operative proliferative vitreoretinopathy (PVR), which increases the risk of redetachment, is believed to be a risk factor for complex redetachment.[13,14] Common techniques used to treat GRTs include pneumatic retinopexy (PR), scleral buckling (SB), primary vitrectomy with gas or silicone oil (SO) tamponade, and combined vitrectomy with complementary scleral buckling.[8] Perfluorocarbon liquids (PFCLs) aid in the management of GRTs. Importantly, the advent of PFCLs as transient or temporary (as short- and medium-term agents) tamponades, the use of medical-grade SO, which has physical advantages such as a buoyancy effect and low interfacial tension, faster-speed cutters, the use of vitrectomy systems with improved fluidics and microincision vitrectomy surgery (MIVS) platforms, and the use of peripheral aberration-free wide-field visualization systems has improved anatomical and functional outcomes.[3,15-18] The final anatomical success rate ranged from 81.8% to 100%.[16] Although the anatomical success rate is high, the final visual outcome may be restricted due to inherent post-operative complications such as the formation of epiretinal membranes (ERMs).[19]
This systematic review aimed to elucidate the functional and anatomical outcomes of surgical approaches and interventions for GRT-associated RRDs, focusing on visual acuity improvement, anatomical success rates, and risk factors. This study also aimed to summarize the diversity of surgical techniques involved in its management. We assessed the effectiveness of various techniques in promoting retinal reattachment and visual rehabilitation. In addition, an analysis of the most frequent complications, such as PVR, macular ERM formation (macular pucker), hypotony, cataracts, endophthalmitis, and foreign body reaction, was conducted.
The findings of this systematic study will serve as a significant asset for retinal surgeons by providing recommendations for selecting the most effective surgical approach and interventions for patients with GRTs. Moreover, it identifies specific locations that require additional examinations, thereby fostering future exploration and advancement in the management of this visually impaired illness.
METHODOLOGY
Search strategy
A systematic literature search was conducted to identify relevant studies published between 2002 and February 2024. Relevant studies were identified through a comprehensive literature search of electronic databases, including PubMed, Embase, Web of Science, and the Cochrane Library. The search strategy included a combination of keywords and Medical Subject Headings (MeSH) terms related to GRTs, surgical approaches, functional outcomes, and complications. The search was limited to studies published in the English language. The detailed keywords and search strategies used were based on the participants, interventions, comparator, outcomes (PICO) framework format, and a free search strategy was used to perform a more comprehensive and accurate search of information sources in different databases, as listed in [Supplementary File]. The reference lists of the included studies and relevant reviews were also screened to identify additional relevant studies.
Study selection criteria
The inclusion criteria for this systematic review were as follows:
Study design: Original research articles, including randomized controlled trials (RCTs), prospective cohort studies, retrospective cohort studies, case reports, and case series, were considered eligible for inclusion. Review articles and editorials were excluded from this study.
Participants: Studies involving adult patients (aged ≥18 years) with GRTs who underwent surgical treatment were included.
Interventions: Studies evaluating various surgical approaches for GRT repair, including three-port pars plana vitrectomy (PPV), and studies using MIVS platforms, SB, combined procedures (PPV with SB), and PR.
Outcome measures: Studies reporting functional outcomes such as visual acuity and anatomical success rates as well as complications associated with surgical approaches, were included.
Timeframe: Studies published between 2002 and February 2024 were included in this systematic review.
Study selection and data extraction
The retrieved articles were screened using the Covidence.org database. Two independent reviewers (Miguel A. QuirozReyes and Erick A. Quiroz-Gonzalez) screened the titles and abstracts of the identified articles for eligibility based on the predefined inclusion criteria. Full-text articles from potentially eligible studies were assessed for final inclusion. Any discrepancies between reviewers were resolved through discussion and consensus. The following data were extracted from the included studies: study characteristics (author, year of publication, and study design), patient characteristics (sample size, age, and sex), number of procedures, surgical approach details, follow-up duration, functional and anatomical outcomes, identified risk factors, and reported complications (retinal redetachment, ERM, PVR, increased intraocular pressure, corneal decompensation, hypotony, foreign body reaction, uveitis, cataracts, and endophthalmitis).
RESULTS
Studies retrieved from database searches
Through electronic searches, we retrieved 4104 unique records, of which 689 were duplicates and 3381 were excluded after screening the titles and abstracts. Thirty-four article abstracts and titles were assessed for eligibility. Twelve studies were excluded for the following reasons: a follow-up period of <6 months, fewer than ten patients, tears with an extent of <90°, or age younger than 18 years. During the screening of the studies, those that did not meet our eligibility criteria also were excluded, resulting in a total of 22 studies[2,3,16,18,20-37] that were selected for full-text screening and synthesis for qualitative analysis in this systematic review [Figure 1]. We contacted the study authors[23,25,26,28,38] in the included studies for further information, but we did not obtain any data from the investigators after waiting for 2 weeks. All included studies were retrospective, and two prospective studies were excluded from the study. The detailed characteristics of the included studies are listed in Table 1.
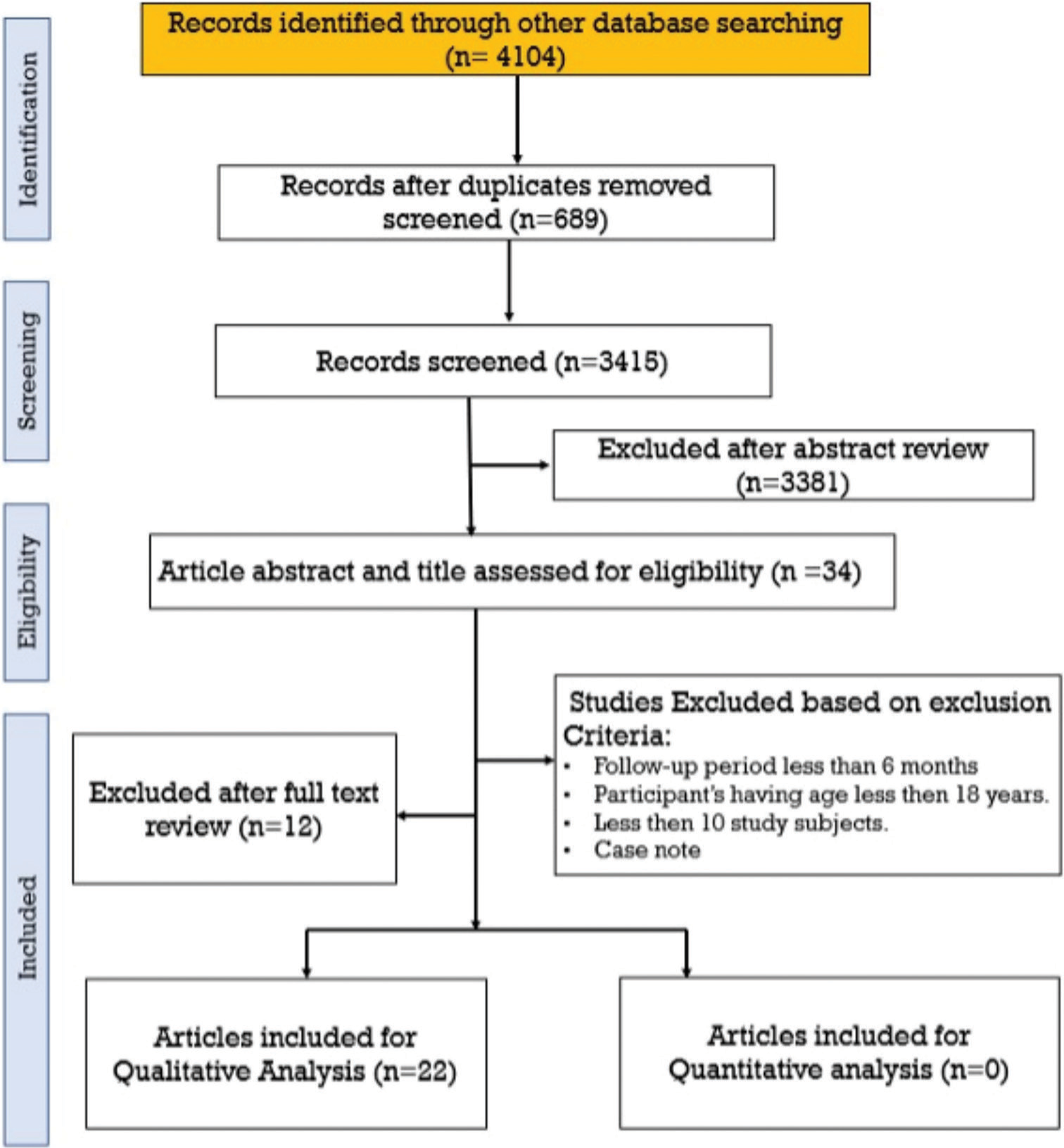
- The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart of the studies included in this systematic review.
| Author and reference number | Number of eyes | Age (years), mean (SD) | Male gender, no. (%) | Study design | Surgical procedure | GRT configuration | Pre-operative visual acuity | Post-operative visual acuity | Follow-Up | Anatomical success |
|---|---|---|---|---|---|---|---|---|---|---|
| Ramamurthy et al., 2022[36] | 240 | 37 years | 339 (86%) | Retrospective | PPV | 277 (70%) eyes had configuration of>180° and<270° | 20/1500 | 20/400 and 15% of eyes achieved post-operative VA of 20/60 or better | 15 months | Anatomical success after initial surgery was 64% (255 eyes), which improved to 78% (308 eyes) after undergoing a second vitreoretinal procedure for recurrent retinal detachment (53 eyes). |
| 152 | PPV+Encircling band | |||||||||
| 4 | PPV+SB | |||||||||
| Ong et al., 2022[25] | 101 | N/A | N/A | Retrospective | PPV | N/A | For both children and adults, the mean BCVA at baseline did not differ between the PPV and PPV/SB groups. | For children, mean BCVA at 1 year was better in the PPV/SB than PPV groups (P=0.001). For adults, no difference was found between the 2 groups. |
12 months | 77.2% |
| 99 | N/A | N/A | PPV+SB | N/A | 85.7% | |||||
| Hocaoglu et al., 2019[34] | 45 | 43.3±13.1 | 37 (84%) | Retrospective | PPV | ≥180° | 1.5±1.3 | 0.46±0.62 | 37.0±34.8 | Overall final reattachment rate was 98% |
| Chang et al., 1989[17] | 23 | 41.7±11.7 | 17 | Retrospective | PPV | range 3–7 clock h | 1.59±0.58 | 0.84±0.51 | 12.2±2.7 | All patients achieved primary anatomic success of 100% |
| Bhardwaj et al., 2020[29] | 19 | 41 years | 18 | Prospective | PPV | 90° to 330° | VA ranges from 20/15 to 20/40 in 5 cases (26%), from 20/60 to 20/200 in 5 (26%), and CF or worse in 9 (48%). | • VA was 20/20 to 20/40 in 11 eyes (58%), 20/60 to 20/200 in 7 (37%), and 20/400 in 1 (5%). • 12 eyes in which the macula was detached, 5 (42%) achieved a final BCVA of 20/40 or better. |
6 months | Final reattachment rate was 100%. |
| Kumar et al., 2018[24] | 17 | 25.7 | 16 | Retrospective review | PPV | >180° | 2.31±1.27 in adults | 0.73 (20/108)±0.38 in adults | 10.1 months | Anatomical success was achieved in 88.2% of eyes (n=15/17) |
| Zgolli et al., 2019[28] | 15 | 45 | Retrospective descriptive study | PPV | 2/10 | 9 months | Immediate post-operative anatomical reapplication was achieved in 85% of patients. After 1-year, anatomical reapplication was achieved in 100% of patients. | |||
| Mikhail et al., 2017[39] | 30 | 43.7 | 23 | Retrospective consecutive case series | PPV | GRTs had a mean size of 150° (range 90–270°) | 1.1 logMAR | 70% had an overall improvement in vision, 42 improved by 2 lines, and 35% had 6/12 vision or better. | 26.8 months | At final follow-up, the anatomic success rate was 27 of 30 eyes (90%). |
| Ghasemi Falavarjani et al., 2017[22] | 44 | 33.96±20.19 | 51 | Retrospective study | PPV | 42 (67.8) have<180 while 20 (32.2) have>180 | 2.47±0.79 logMAR | 1.43±0.92 logMAR | 21.54±27.73 | Anatomic success after one vitrectomy procedure was achieved in 45 eyes (72.58%) and ultimately in 61 eyes (98.4%) at last follow up. |
| 7 | Encircling episcleral band (The reason for placing the episcleral band was the age (≤18 years) in 4 eyes) | |||||||||
| 18 | PPV and phacoemulsification surgery | VA improved in 70% | ||||||||
| Al-Khairi et al., 2008[16] | 117 | 30.3±15.2 | 93 | Retrospective study | PPV was performed in all eyes and PPV with encircling buckle was performed in 90 eyes | • 90–180 in 54.4% • >180° in 44.4% |
20/200 | VA improved in 17.9% from 20/200 | 29.7±26.7 | Success rate with primary procedure was 78.6%, which increased to 94% with multiple surgeries. |
| Goezinne et al., 2008[18] | 30 | 53.2 | 26 | Retrospective | PPV and PPV with encircling SB was placed in 21 eyes (70%) | • 18 eyes have 3 clock h. • 12 eyes have>4 clock h. |
15 eyes have 0.1 while the rest 15 have >15 eyes | 13 eyes (43.3%) had a VA of 0.1 or less. VA improved in 54% of the eyes. | 49 months | Single operation success is 70% and Final success was 96.4% |
| Lee et al., 2009[30] | 99 | 39.6 years | 113 | Retrospective | PPV in all eyes and PPV with encircling SB was performed in 90 eyes | - | - | 41 eyes (41.4%) regained 20/40 or better vision. Surgical success for GRT can be achieved with a good visual outcome in 84.8%. | 63.38 months | Single operation success was 71.7% and final success was 84.8% |
| Jain et al., 2014[23] | 41 | - | - | Retrospective | PPV | - | - | VA improved in 59% | - | Final success was 75% |
| Pitcher III et al., 2015[26] | 54 | 52 | - | Retrospective | PPV alone was performed in all eyes and PPV with SB was placed in 30 eyes (52%) | - | 20/500 | 20/88 | 17 months, | Single operation success was 88% and Final success was 100%. |
| Dabour, 2014 [35] | 24 | 37.1±10.6 | 19 | Prospective | PPV with encircling SB | GRT>180 | Pre-operative BCVA ranged from HM to CF in macula-off patients, while decimal BCVA in eyes with attached macula was 0.15 in two eyes and 0.05 in one eye. | BCVA improved in 21 (87.5%) eyes, did not change in two (8.3%) eyes, and worsened in one (4.2%) eye. | 13.7±6.5 | Final success was 83.3%. |
| Gonzalez et al., 2013[37] | 79 | 43.7 | 64 | Retrospective | All 79 eyes underwent PPV during initial reattachment surgery [Figures 2 and 3]. An encircling SB was utilized in 67 eyes (85%), | The GRT was 90° in 31 eyes (39.2%), >90° but<180° in 30 eyes (37.9%), and≥180° in 18 eyes (22.8%) | • ≥20/40 in 26 eyes (33%). • <20/400 in 48 eyes (61%). • <20/400 in 31 eyes (39%). |
• VA was≥20/40 in 17 eyes (22%). • >20/400 in 58 eyes (73%). • >20/400 in 21 eyes (27%). • VA improved in 57% |
20.4 | Final success was 94.9% |
| Eiger-Moscovich et al., 2017[40] | 13 | 54±12 | 11 | Retrospective | PPV | - | - | The final BCVA was equal to or better than 20/100. | 11±11 | 6 (60%) had a final BCVA that was equal to or better than the initial BCVA |
| Randolph et al., 2016[33] | 23 | 50.47±11.12 | 19 | Retrospective | PPV and MT-PFO. | Large retinal break with circumferential measurement of≥90°, or≥3 clock-h | 1.01±0.75 logMAR | 1.08±0.81 logMAR | 33.04±19.74 | Successful reattachment was achieved in 91.3% of eyes (21/23) after MT-PFO. Anatomic reattachment was achieved in 91.3% (n=21) of cases after initial staged surgery. |
| Sirimaharaj et al., 2005[31] | 62 | 44.2 | 51 | Retrospective | PPV | • 90–180° in 45 • 180°–270° in 16>270° in 1 |
• 6/6–6/12 in 25 eyes • 6/15–6/24 in 1 • 6/36–6/60 in 4 • 6/120 in 3 • CF<<f in 11 • HM in 13 • LP in 5 |
• VA 6/12 or better in 27 eyes (46.5%). • The VA improved in 34 eyes (54.8%) with 28 eyes (45.2%) improving at least two Snellen lines, it was unchanged in 20 eyes (32.3%), and was worse in eight eyes (12.9%). |
24.5 months | At final visit, 58 eyes (93.5%) had retinas that remained attached. |
| Ambresin et al., 2003[21] | 18 | 43.9 years | 13 | Retrospective | PPV | • The GRT was 180 degrees or greater in seven eyes. • 90 degrees to 180 degrees in 11 eyes. |
N/A | • VA improved in 9 of the 16 eyes. • Remained unchanged in four eyes, and decreased in three eyes |
28.6 | The retina was attached in 17 (94.4%) of the 18 eyes. |
| Ünlüet al., 2003[32] | 21 | 33.5 years | 17 | Retrospective | PPV | • Fourteen eyes (66.7%) had GRT between 90° and 180°. • 7 eyes (33.3%) had tears>180° |
VA ranged from 20/40 to light perception | Final VA was equal to or better than 20/200 in 7 eyes (33.3%). VA improved in 15 eyes (71.4%) | 12.5 months | Retinal attachment was obtained in 17 (80.5%) of 21 eyes. |
| Scott et al., 2002[3] | 212 | 41 | 160 | Prospective | PPV in all and PPV with SB was performed in 131 (62%). | • The GRT was 90° in extent in 24 (14%) patients. • >90° in 152 (86%) patients. • >180° in 41 (23%) patients |
• 20/80 in 43 (21) • 20/80–20/200 in 13 (6) • 20/400 in 10 (5) • 5/200–CF in 49 (24) • HM, light perception in 91 (44) • No light perception 1 (1) |
• 20/200 or better was measured in 67 (47%) patients. | 3.8 months | Post-operative visual acuity improved in 107 (59%) eyes, remained stable in 44 (24%) eyes, and worsened in 29 (16%) eyes. |
BCVA: Best -corrected visual acuity, CF: Counting fingers, GRT: Giant retinal tear, HM: Hand motion, logMAR: Logarithm of the minimum angle of resolution, N/A: Not applicable, PPV: Pars plana vitrectomy, MT -PFO: Medium -term post -operative perfluoro -n -octane, SB: Scleral buckling, VA: Visual acuity, SD: Standard deviation
Post-operative visual outcomes
The primary focus of this systematic review was adults. Most of the included studies investigated and reported GRT-associated RRD in adults, whereas other studies compared adults with children.[25] A total of 1607 patients were included in the studies, 1087 of whom were male; however, Jain et al., Ong et al., Pitcher et al., and Zgolli et al.[23,25,26,28] did not provide sex information. After excluding 300 participants, among the 1297 study subjects, 1087 (83.8%) were male. This systematic review showed that GRT-associated RRD was more prevalent in males than in females. Post-operative best-corrected visual acuity (BCVA) varied across studies, with outcomes reported in different formats, such as Snellen lines or LogMAR units. Notably, there are a range of visual improvements, and some studies have highlighted specific improvements in visual acuity [Table 1]. Randolph et al.[33] reported that the pre-operative BCVA ranged from hand motion to counting fingers and that the BCVA improved in 87.5% of the eyes; however, the number of samples was quite low. Mikhail et al.[39] reported a 70% overall improvement in vision, with 42% improvement by two lines and 35% achieving 6/12 vision or better. Bhardwaj et al.[29] reported visual acuity ranging from 20/15 to 20/40 in 26% of cases, 20/60 to 20/200 in 37%, and counting fingers or worse in 48% of patients after using a single surgical procedure involving PPV alone. According to Ramamurthy et al.,[36] visual acuity improved from 20/1500 to 20/400, and 15% of the eyes achieved a post-operative visual acuity of >20/60 after a combination of PPV and SB. Interestingly, Ong et al.[25] reported that, in children, visual acuity improved and was better in the PPV/SB group than in the PPV group (P = 0.001); however, in adults, no differences were observed between the two groups. The included studies on GRTs indicated a spectrum of post-operative visual improvements, with most studies showing positive outcomes after PPV. Although the degree of improvement varies, the evidence suggests that age may influence visual success.
When evaluating functional and anatomical outcomes and complication rates, several risk factors were identified, including age, pre-operative presence of PVR, timing of surgery, pre-operative status of the macula, number of detached retinal quadrants, myopia, male sex, and more than 150° of GRT extension.[2-6,13,16,22,24,35-37]
Post-operative anatomical outcomes
However, anatomical success rates after surgical intervention for GRTs have varied among studies. The initial anatomical success rates ranged from 70% to 100%. PPV was the most common surgical procedure performed in all the reviewed studies [Table 2]. PPV has been associated with varying degrees of success in achieving anatomical reattachment. Several studies have included additional surgical interventions, such as SB or the use of an episcleral band, with positive outcomes in terms of anatomical success. The postoperative anatomical outcomes of the included studies varied, reflecting the complexity of managing GRT-associated RRDs. Ramamurthy et al.[36] reported a 78% anatomical success rate after a second vitreoretinal procedure, followed by an initial success rate of 64%. Ong et al.[25] reported a 77.2% success rate after 12 months, with better outcomes in children undergoing PPV with SB. According to Hocaoglu et al.,[34] the overall final reattachment rate is 98%, whereas Chang et al.[17] and Bhardwaj et al.[29] reported 100% anatomical success. Furthermore, Kumar et al.[24] achieved anatomical success in 88.2% of eyes, whereas Falavarjani et al.[22] noted anatomical success in 72.58% of eyes after one vitrectomy, which increased to 98.4% at the last follow-up. Overall, these studies demonstrated variable success rates, with some reports achieving high rates of anatomical success, especially with multiple surgeries, highlighting the challenges and nuances in managing GRT-associated RRDs.
| Surgical procedure | Number of eyes | Prevalence (%) |
|---|---|---|
| PPV alone | 1073 | 80.30 |
| PPV+Encircling band | 159 | 11.92 |
| PPV+Scleral buckle | 103 | 7.72 |
GRT: Giant retinal tear, RRD: Rhegmatogenous retinal detachment, PPV: Pars plana vitrectomy
Post-operative complications
Analysis of post-operative complications revealed various outcomes [Table 3]. Encircling SB appears to decrease the risk of recurrent RD according to Al-Khairi et al.[16] Ramamurthy et al.[36] emphasized the factors leading to poor anatomical success in patients with a visual acuity ≤20/400 and in those aged <16 years. PVR is a major cause of redetachment according to Ang et al.[5] and Ong et al.)[25] PPV with PFCL as a short-term tamponade is effective in repairing GRT, but it leads to complications such as a foreign body reaction and cataracts, as observed in studies by Zhang et al., Ambresin et al., Eiger-Moscovich et al., Mikhail et al., and Sirimaharaj et al.[20,21,31,39,40] Bhardwaj et al.[29] highlighted cataract formation as a major complication of transscleral diode laser retinopexy using perfluoro-n-octane (PFO) for short-term post-operative tamponade. Overall, these studies underscore the efficacy of different surgical approaches, emphasizing the need for careful consideration of complications such as cataracts, foreign body reactions, and anatomical success factors in managing GRT-associated RRDs.
| Author and reference number | Recurrent RD and post-operative PVR | Multiple operations | Raised IOP | Hypotony | Corneal decompensation | Uveitis | Cataract | Macular pucker | Foreign body response | Endophthalmitis | Comment |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Al-Khairi et al., 2008[16] | 25 (21.4%) | 25 (21.4%) | 24 (20.5%) | 1 (0.9%) | N/A | N/A | 23 of 33 (70%) | N/A | N/A | N/A | Encircling SB decreased the risk of recurrent RD |
| Ramamurthy et al., 2022[36] | 53 (13.38%) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | The factors that lead to poor anatomical success in study participants presenting VA 20/400 or less and age<16 years. |
| Ong et al., 2022[19] | PVR was the major cause for redetachment (70.4% of PPV and 93.8% of PPV/SB in redetached eyes). However, the exact figure of RRD N/A. | N/A | N/A | N/A | N/A | N/A | They observed cataract after surgical operation, but the exact figure is not mentioned. | N/A | N/A | N/A | In adults, the GRT's alleviation of traction may decrease peripheral traction, eliminating the necessity for SB |
| Zhang et al., 2018[20] | N/A | N/A | 5 (21.7%) | N/A | N/A | N/A | 11 (70.6%) | N/A | 7 (30%) | N/A | PPV with PFCL tamponade is effective for the repair of GRT, but it leads to foreign body response and cataract, which is its major side effect. |
| Ambresin et al., 2003[21] | 2 (11.1%) | 2 (11.1%) | 1 (5.6%) | N/A | N/A | N/A | 5 of 8 (63%) | 1 (5.6%) | N/A | N/A | PPV with PFCL tamponade is effective but cataract is a major complication. |
| Hocaoglu et al., 2019[34] | 7 (16%) | 8 (18) | 10 (22) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | The substantial anatomical and functional success underscores the efficacy of managing GRTs through vitrectomy alone, without the need for additional SB. Timely removal of SO is crucial to prevent complications like keratopathy, glaucoma, and unexplained visual loss. |
| Ang et al., 2009[5] | 12 (21%) | 12 (21%) | 16 (28%) | N/A | N/A | 3 (5.3%) | 31 of 44 (71%) | 8 (14%) | N/A | 0 | |
| Bhardwaj et al., 2020[29] | 3 (15%) | N/A | N/A | N/A | N/A | N/A | 6 (31%) | 2 (10%) | N/A | N/A | Transscleral diode laser retinopexy together with PFO as a post-operative short-term tamponade achieved good anatomical result but it leads to the formation of cataract, a major complication. |
| Dabour, 2014[35] | N/A | N/A | N/A | N/A | N/A | N/A | 14 (58%) | N/A | N/A | N/A | Treating RD with a>180° extent is effectively achieved through a combination of PPV along with encircling SB, 360° laser retinopexy, and SO tamponade. This comprehensive approach minimizes the risk of retinal slippage, and the use of concurrent encircling SB during the primary intervention enhances the likelihood of success. However, it is important to note that cataract formation represents a significant complication in this complex procedure. |
| Eiger-Moscovich et al., 2017[40] | N/A | N/A | 2 (15%) | N/A | N/A | N/A | 2 (15%) | N/A | N/A | N/A | PPV with PFCL tamponade is effective but cataract is a major complication. |
| Goezinne et al., 2008[18] | 9 (30%) | N/A | 1 (3.3%) | N/A | 1 (3.3%) | N/A | 21 (Insufficient data) | N/A | N/A | 1 (3.3%) | PPV with SB might be a preferred treatment for complicated retinal RDs due to GRT |
| Ghasemi Falavarjani et al., 2017[22] | 17 (27.4%) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Impressive findings with a 72.58% single-operation success rate and a remarkable 98.4% final anatomic success rate in our study. These results underscore the potential for high surgical success in both single and multiple surgeries for nearly all patients. |
| Lee et al., 2009[30] | 15 (15.2%) | 0.131 | 4 (3.1%) | N/A | 1 (0.8%) | N/A | 17 (Insufficient data) | N/A | N/A | N/A | Surgical management using PPV, and SB have enhanced the prognosis of managing GRTs, resulting in an 84.8% success rate with favorable visual outcomes after a mean of 1.19 surgeries. Notably, 70.7% of eyes achieved 6/60 or better acuity at 6 months, suggesting improved functional outcomes, but careful observation and long-term follow-up are recommended for fellow eyes, especially in cases with lattice degeneration and retinal breaks. |
| Gonzalez et al., 2013[37] | 14 (18%) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | This study highlights improved anatomic, single surgery success of eyes with GRT and better final visual results, that is a result of without any complications. |
| Scott et al., 2002[3] | 64 (30%) | N/A | 6 (3%) | N/A | N/A | N/A | 61 of 73 (84%) | N/A | N/A | The study on GRT management using intraoperative PFO suggests that the approach is generally effective in achieving retinal reattachment and preserving VA, with notable risk factors for recurrent detachment being the size of GRT, age, prior vitrectomy, and female gender. | |
| Jain et al., 2014[23] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Insufficient data |
| Mikhail et al., 2027[39] | N/A | N/A | 2 (6%) | N/A | N/A | 6 (20%) | 15 (50%) | N/A | N/A | N/A | PPV with PFCL tamponade is effective but cataract is a major complication. |
| Kumar et al., 2018[24] | N/A | N/A | N/A | N/A | N/A | N/A | 4 (23.5%) | None | N/A | None | PPV can achieve excellent attachment rates and least post-operative complications in eyes with GRT–associated RD. |
| Pitcher III et al., 2015[26] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Insufficient data |
| Sirimaharaj et al., 2005[31] | 13 (21.0%) | 13 (21.0%) | 3 (4.8%) | N/A | N/A | N/A | 29 of 36 (81%) | N/A | N/A | N/A | PPV with PFCL tamponade is effective but cataract is a major complication. |
| Randolph et al., 2016[33] | N/A | N/A | 8 (34.8 %) | N/A | N/A | N/A | 10 (44%) | N/A | 7 (30.4 %) | N/A | The study finds that PPV with post-operative MT-PFO is effective and safe for treating GRTs, resulting in successful reattachment in 91.3% of cases. However, potential complications such as cataract progression and transient IOP elevation may affect visual outcomes. |
| Ünlüet al., 2003[32] | 3 (14.3%) | 3 (14.3%) | 3 (14.3%) | N/A | 1 (4.7%) | N/A | 7 of 11 (64%) | 2 (9.5%) | N/A | N/A | PPV with SO tamponade seems highly effective in GRTs anatomical and functional outcomes, but cataract is the major side effect. |
| Zgolli et al., 2019[28] | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A | Insufficient data |
GRT: Giant retinal tear, IOP: Intraocular pressure, N/A: Not applicable, PFCL: Perfluorocarbon liquid, PFO: Perfluoro -n -octane, PVR: Proliferative vitreoretinopathy, PPV: Pars plana vitrectomy, MT -PFO: Medium -term post -operative perfluoro -n -octane, RD: Retinal detachment, SB: Scleral buckling, SO: Silicone oil, VA: Visual acuity
DISCUSSION
A search of the relevant literature on the management of GRTs led us to explore various electronic databases to identify studies that assessed the efficacy of different surgical procedures in addressing this complex condition. Despite the significance of GRTs in ophthalmic pathology, we encountered a predominance of retrospective reports and case series in the published literature. Our main objective was to thoroughly examine the extensive and rigorous evidence, specifically focusing on randomized and comparative studies that could provide insights into the comparative effectiveness of different surgical treatments.
To compensate for the scarcity of RCTs and prospective literature on the subject, we expanded our search parameters and selection criteria to encompass pertinent papers published from 2002 onward. Through strategic expansion, we were able to gather a thorough summary of the current literature on GRT management, although it mostly consisted of retrospective and case series research. By adopting this method, we were able to include and examine the existing data, providing valuable insights into the status of research on the management of GRTs during the past 22 years. Furthermore, this study revealed promising areas for future research on surgical therapy for GRTs.
GRT-associated RRDs are uncommon and complex vitreoretinal disorders with a high incidence of potential surgical and inherent complications, which frequently lead to additional surgical procedures and poor functional recovery.[38] Most available research data originate from nonrandomized studies, with reported primary retinal reattachment rates ranging from 71.7% to 100%.[3,6,18,21,24,27,29,30,41] However, 100% final reattachment was achieved by Bhardwaj et al.[29] in a small number of patients. In contrast, Ramamurthy et al.[36] reported anatomical success in 64% (255 eyes) of eyes after primary surgery, which improved to 78% (308 eyes) after a second vitreoretinal procedure for recurrent RD (53 eyes); the observed variability in anatomical success may be affected by patient age.[42] Additional factors that should be examined in future well-blinded RCTs include the extent of GRT, post-operative tamponade selection,[32] necessity of adjunctive scleral buckling,[34,38] use of transscleral diode laser retinopexy,[29] severity of pre-operative PVR as a main risk factor for anatomical failure,[36] significance of extensive pre-operative choroidal detachment,[43] and application of PFO as a short- or medium-term post-operative tamponade.[31,33,39,44,45]
The main problems observed in a thorough examination of the studies that used PFO as a temporary tamponade were cataracts and foreign body reactions. Significantly, postoperative cataract formation has emerged as a significant concern, and its association with the use of PFCL tamponade has been consistently observed in multiple studies. This observation aligns with previous research,[43] which established a significant association between PFCL use and diverse post-operative complications, including hypotony, macular detachment, and cataract development. Moreover, two distinct studies[20,33] reported significant foreign body reactions associated with the use of PFO as a short- or medium-term post-operative tamponade. Randolph et al.[33] reported that the incidence of foreign body reactions was 30.4%, which was substantially greater than that reported in previous clinical trials that used post-operative PFO for retinal detachment.[44,45] These findings highlight the importance of thoroughly considering and evaluating the use of tamponade agents in retinal procedures, particularly for PFCLs. The difficulties that have been observed, specifically the development of cataracts after surgery and foreign body reactions, highlight the importance of continuously improving surgical techniques and maximizing patient outcomes. These observations enhance our overall understanding of the complexities involved in selecting tamponade options for retinal surgeries and lay the groundwork for future research efforts focused on improving the safety and effectiveness of these procedures.
According to functional and final anatomical evaluations, PVR was the most frequently identified risk factor for disappointing results, followed by circumferential extension of more than 150° of the GRT, low pre-operative visual acuity, pre-operative macular status, the number of detached retinal quadrants, myopia, and age.[2-6,13,16,22,24,35-37]
In summary, it is currently unclear whether there are any possible benefits to treating GRTs by adding an encircling SB and eliminating the advantages of MIVS in selected cases. In line with our research, several studies have discussed the challenge of assessing whether the use of a scleral buckle in conjunction with PPV in GRT surgery can negatively impact the outcomes of the procedure. Due to the absence of information for assessing the risk of bias and inconclusive data from RCTs, it is challenging to draw conclusions from non-randomized research because patient characteristics and the comparability of surgical procedures cannot be determined.[19,38]
The following are some recommendations for choosing the best surgical strategy and therapy for patients with GRTs, as revealed by the extensive analysis in this study. The most effective surgical technique is the use of 25- or 27-gauge MIVS systems regardless of the extent of the GRT; the placement of complementary scleral buckling is reserved for specially selected patients, such as those with an inferior GRT complicated with severe primary PVR or redetachment with severe anterior PVR; primary PR is rarely used and is indicated for selected superior GRTs without vitreous traction or PVR; the most widely used tamponade is SO; and PFO is safe for use as a temporary tamponade for short or medium periods of time.
This systematic review had several limitations. The main constraint lies in the lack of definitive information obtained from RCTs, which might present difficulties for ophthalmologists when making well-informed judgments to achieve better anatomical outcomes and lower surgical failure rates. Furthermore, research examining past events or studies that are not randomized and lack proper planning is insufficient to answer these questions. Therefore, it is crucial to conduct well-designed RCTs to evaluate the relative benefits of various modern surgical techniques for the treatment of GRTs. One of the main obstacles to making appropriate decisions regarding GRT approaches is the lack of comparative data on surgical techniques for conducting meta-analyses. To address the significant obstacle posed by the lack of comparative data on surgical techniques for GRTs, we recommend conducting well-designed RCTs and establishing a comprehensive, standardized database to facilitate robust meta-analyses. However, it is crucial to provide meticulous post-operative care to address any issues that may arise postoperatively. Despite these limitations, our study showed that when combined with meticulous post-operative care to address post-operative issues, MIVS-based PPV is currently the optimal approach for treating GRTs in adults to improve anatomical and visual results.
CONCLUSION
This systematic review provides a thorough examination of surgical procedures and interventions, highlighting that PPV using 25- and 27-gauge MIVSs is currently the most advantageous surgical method for treating GRT in adults. The findings highlight the variation in visual outcomes after surgery, the success rates in terms of anatomical results, and problems linked to different surgical methods. The prevalence of GRT in males and the influence of age on the effectiveness of surgery emphasize the significance of patient-specific factors. Although anatomical success rates may vary, the occurrence of problems such as PVR, macular pucker, cataract formation, and foreign body reaction highlights the significance of meticulous post-operative care. Additional research and innovation are required to address the gaps and limitations mentioned in the literature and improve the understanding and management of these intricate conditions.
Supplementary information
Photographs and tables from this study may be released via a written application to the Photographic Laboratory and Clinical Archives of the Retina Department of Oftalmologia Integral ABC, Nonprofit Medical and Surgical Assistance Institution Av. Paseo de las Palmas 735 suite 303, Lomas de Chapultepec, Mexico City 11,000, Mexico, and the corresponding author upon request. The search strategy file can be found in the Supplementary Information.
Data availability statement
The datasets used in this study have been included in the main text. Images, figures, and tables from this study may be released via a written application to the Photographic Laboratory and Clinical Archives Retina Department of Oftalmologia Integral ABC (Nonprofit Medical and Surgical Organization), Av. Paseo de las Palmas 735 suite 303, Lomas de Chapultepec, Mexico City 11000, Mexico and the corresponding author on request.
Acknowledgments
We express our deep appreciation to the technical staff of the Retina Department of Oftalmologia Integral ABC (Nonprofit Medical and Surgical Organization), Mexico City, Mexico, which is affiliated with the Postgraduate Studies Division of the National Autonomous University of Mexico.
Authors contributions
MAQR: study conception, study design, countercheck, manuscript writing, final revision, data extraction, selection process, statistical analysis, study quality assessment, writing of the draft, and data extraction; EAQG: tables, photographic material compilation, and draft revision; MAQG: PRISMA flow chart, and tables; VLG: statistical check, final revision. All the authors have approved the manuscript for submission.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Retinal detachments with giant breaks: Preliminary report. Trans Am Acad Ophthalmol Otolaryngol. 1962;66:471-9.
- [Google Scholar]
- Epidemiology of giant retinal tears in the United Kingdom: The British giant retinal tear epidemiology eye study (BGEES) Invest Ophthalmol Vis Sci. 2010;51:4781-7.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes and complications associated with giant retinal tear management using perfluoron-octane. Ophthalmology. 2002;109:1828-33.
- [CrossRef] [PubMed] [Google Scholar]
- The epidemiology of rhegmatogenous retinal detachment: Geographical variation and clinical associations. Br J Ophthalmol. 2010;94:678-84.
- [CrossRef] [PubMed] [Google Scholar]
- Interventions for prevention of giant retinal tear in the fellow eye. Cochrane Database Syst Rev. 2009;2:CD006909.
- [CrossRef] [Google Scholar]
- Surgical treatment and outcome of patients with giant retinal tears. Eye. 2004;18:996-1000.
- [CrossRef] [PubMed] [Google Scholar]
- Adjuvant 5-fluorouracil and heparin prevents proliferative vitreoretinopathy: Results from a randomized, double-blind, controlled clinical trial. Ophthalmology. 2001;108:1179-83.
- [CrossRef] [PubMed] [Google Scholar]
- Age-related changes on the surface of vitreous collagen fibrils. Invest Ophthalmol Vis Sci. 2004;45:1041-6.
- [CrossRef] [PubMed] [Google Scholar]
- Rhegmatogenous retinal detachments in children: Risk factors and surgical outcomes. Ophthalmology. 2003;110:1708-13.
- [CrossRef] [PubMed] [Google Scholar]
- Pediatric rhegmatogenous retinal detachment: Clinical features and surgical outcomes. Retina. 2008;28:847-52.
- [CrossRef] [PubMed] [Google Scholar]
- Retinal detachment in East Africa. Ophthalmology. 2002;109:2279-83.
- [CrossRef] [PubMed] [Google Scholar]
- Characteristics of primary rhegmatogenous retinal detachment in Taiwan. Eye. 2007;21:1056-61.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of giant retinal tears combined with proliferative vitreoretinopathy. Ophthalmology. 1986;93:1193-7.
- [CrossRef] [PubMed] [Google Scholar]
- Giant retinal tears: Clinical features and outcomes of vitreoretinal surgery at a university teaching hospital (2011-2017) Clin Ophthalmol. 2018;12:2053-8.
- [CrossRef] [PubMed] [Google Scholar]
- Low viscosity liquid fluorochemicals in vitreous surgery. Am J Ophthalmol. 1987;103:38-43.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic factors associated with outcomes after giant retinal tear management using perfluorocarbon liquids. Eur J Ophthalmol. 2008;18:270-7.
- [CrossRef] [PubMed] [Google Scholar]
- Giant retinal tears: Surgical techniques and results using perfluorocarbon liquids. Arch Ophthalmol. 1989;107:761-6.
- [CrossRef] [PubMed] [Google Scholar]
- Low redetachment rate due to encircling scleral buckle in giant retinal tears treated with vitrectomy and silicone oil. Retina. 2008;28:485-92.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical outcomes of 27-gauge pars plana vitrectomy with short-term postoperative tamponade of perfluorocarbon liquid for repair of giant retinal tears. Int Ophthalmol. 2018;38:1505-13.
- [CrossRef] [PubMed] [Google Scholar]
- Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 retinal photocoagulation. Retina. 2003;23:622-8.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of surgery in patients with giant retinal tear: 10 years experience. Eye. 2017;31:1284-9.
- [CrossRef] [PubMed] [Google Scholar]
- Vitrectomy alone in the management of giant retinal tears. Ophthalmic Surg Lasers Imaging Retina. 2014;45:421-7.
- [CrossRef] [PubMed] [Google Scholar]
- Twenty-five-gauge pars plana vitrectomy in complex retinal detachments associated with giant retinal tear. Retina. 2018;38:670-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vitrectomy versus vitrectomy with scleral buckling in the treatment of Giant Retinal tear related retinal detachments: An International multicenter study. Ophthalmol Retina. 2022;6:595-606.
- [CrossRef] [PubMed] [Google Scholar]
- Contemporary management of rhegmatogenous retinal detachment due to giant retinal tears: A consecutive case series. Ophthalmic Surg Lasers Imaging Retina. 2015;46:566-70.
- [CrossRef] [PubMed] [Google Scholar]
- Lens-sparing vitrectomy with perfluorocarbon liquid for the primary treatment of giant retinal tears. Ophthalmology. 1995;102:17-20.
- [CrossRef] [PubMed] [Google Scholar]
- The results of vitrectomy in giant tear retinal detachments. Tunis Med. 2019;97:1268-71.
- [Google Scholar]
- Management of giant retinal tears using transscleral diode laser retinopexy and short-term postoperative tamponade with perfluoro-n-octane. Retina. 2020;40:546-51.
- [CrossRef] [PubMed] [Google Scholar]
- Giant retinal tear management: An Asian experience. Eye. 2009;23:601-5.
- [CrossRef] [PubMed] [Google Scholar]
- Vitrectomy with short term postoperative tamponade using perfluorocarbon liquid for giant retinal tears. Br J Ophthalmol. 2005;89:1176-9.
- [CrossRef] [PubMed] [Google Scholar]
- The management of giant retinal tears with silicone oil. Eur J Ophthalmol. 2003;13:192-5.
- [CrossRef] [PubMed] [Google Scholar]
- 25-gauge pars plana vitrectomy with medium-term postoperative perfluoro-n-octane for the repair of giant retinal tears. Graefes Arch Clin Exp Ophthalmol. 2016;254:253-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vitrectomy with silicone oil tamponade for retinal detachment associated with giant retinal tears: Favorable outcomes without adjuvant scleral buckling. Acta Ophthalmol. 2019;97:e271-6.
- [CrossRef] [Google Scholar]
- The outcome of surgical management for giant retinal tear more than 180. BMC Ophthalmol. 2014;14:86.
- [CrossRef] [PubMed] [Google Scholar]
- Giant retinal tear detachment: Clinical presentation and treatment outcomes in 396 patients. Retina. 2023;43:784-92.
- [CrossRef] [PubMed] [Google Scholar]
- Surgery for retinal detachment in patients with giant retinal tear: Etiologies, management strategies, and outcomes. Ophthalmic Surg Lasers Imaging Retina. 2013;44:232-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pars plana vitrectomy combined with scleral buckle versus pars plana vitrectomy for giant retinal tear. Cochrane Database Syst Rev. 2019;12:CD012646.
- [CrossRef] [PubMed] [Google Scholar]
- Management of giant retinal tears with vitrectomy and perfluorocarbon liquid postoperatively as a short-term tamponade. Eye. 2017;31:1290-5.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term vitreoretinal tamponade with heavy liquid following surgery for giant retinal tear. Curr Eye Res. 2017;42:1074-8.
- [CrossRef] [PubMed] [Google Scholar]
- Vitrectomy with silicone oil or long-acting gas in eyes with giant retinal tears: Long-term follow-up of a randomized clinical trial. Retina. 1999;19:188-92.
- [CrossRef] [PubMed] [Google Scholar]
- The management of giant retinal tears using perfluoroperhydrophenanthrene: A multicenter case series. Ophthalmology. 1997;104:1159-65.
- [CrossRef] [PubMed] [Google Scholar]
- Perfluoro-n-octane as a postoperative vitreoretinal tamponade in the management of giant retinal tears. Retina. 2005;25:897-901.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term intraocular tamponade with perfluorocarbon heavy liquid. Br J Ophthalmol. 2011;95:694-8.
- [CrossRef] [PubMed] [Google Scholar]







