Translate this page into:
Long-term efficacy of perceptual learning therapy in amblyopia: A 5-year follow-up study

*Corresponding author: Damaris Magdalene, Department of Paediatric Ophthalmology Service and Squint Service, Sri Sankaradeva Nethralaya, Guwahati, Assam, India. drmaggie01@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Magdalene D, Dutta P, Blah P, Sharannya TR, Sharma R, Nath RP, et al. Long-term efficacy of perceptual learning therapy in amblyopia: A 5-year follow-up study. Lat Am J Ophthalmol. 2025;8:8. doi: 10.25259/LAJO_2_2025
Abstract
Objectives
This study aimed to evaluate the long-term outcomes of amblyopic patients treated with perceptual learning therapy (PLT) over a 5-year follow-up period, focusing on visual acuity improvements, binocular function restoration, and the sustainability of therapeutic effects.
Material and Methods
A prospective observational study was conducted at a tertiary eye care center, enrolling 89 amblyopic patients who had achieved maximum visual improvement through optical correction and patching. Participants underwent 30–40 sessions of PLT using RevitalVision software, with training conducted at home. Visual perceptual tasks were performed using Gabor patches to enhance contrast sensitivity and spatial resolution. Visual acuity was assessed at baseline and 1, 2, 3, and 5 years.
Results
Visual acuity showed significant improvement between baseline and 1-year, 2-year, and 3-year visits, with gradual improvement observed over time. The mean visual acuity on LogMAR chart improved from 0.56 ± 0.27 at presentation to 0.30 ± 0.24 beyond 3 years. Amblyopia types included refractive (89.87%), deprivation (2.25%), strabismic (4.49%), and combined mechanism (3.37%). Improvement was observed in 83% of participants, with significant results for both unilateral and bilateral amblyopia (p < 0.001). Notably, age did not significantly affect the visual acuity improvement.
Conclusion
PLT significantly improves visual acuity in amblyopic patients and provides sustained benefits over a 5-year follow-up period. The findings support the use of PLT as an effective alternative treatment for amblyopia, particularly for individuals with residual deficits after traditional interventions. Further studies are needed to explore its broader clinical applications and long-term effects.
Keywords
Amblyopia
Neurodevelopement
Perceptual learning therapy
INTRODUCTION
Amblyopia, commonly referred to as “lazy eye,” is a neurodevelopmental disorder characterized by reduced visual acuity in one or both eyes that cannot be attributed to structural abnormalities of the eye itself. It typically arises from abnormal visual experiences during early childhood, such as strabismus, anisometropia, or form deprivation, which disrupts the development of normal binocular vision. The condition affects approximately 2–4% of the population, posing a significant public health concern due to its impact on visual function and quality of life.[1] Early diagnosis and intervention are critical, as the visual system exhibits heightened plasticity during childhood.[1] If left untreated, amblyopia can lead to permanent visual deficits, including impaired depth perception and reduced contrast sensitivity.[1] Studies have also demonstrated that cortical deficits, particularly in the primary visual cortex, contribute to the condition’s pathophysiology.[2] Kiorpes and Daw highlighted that amblyopia results from altered synaptic connections and reduced neural responsiveness, leading to monocular suppression and cortical reorganization.[2]
Traditional treatments for amblyopia, including patching and atropine penalization, have demonstrated variable success, particularly in older children and adults.[3] Brin et al. conducted a meta-analysis of randomized controlled trials, revealing that traditional methods often fail to address residual visual deficits and are associated with low compliance rates.[3] These findings underscore the need for alternative therapeutic strategies capable of leveraging neural plasticity beyond the critical period.[3] Recent advances have focused on PLT as an emerging approach to treating amblyopia by exploiting the brain’s capacity for experience-dependent plasticity.[4] Levi and Li described PLT as a process involving repetitive practice of visual tasks designed to improve contrast sensitivity, spatial resolution, and visual acuity.[4] Studies have demonstrated that PLT induces neural changes in the visual cortex, enhancing synaptic efficiency and facilitating visual recovery.[4] Magdalene et al. further highlighted the efficacy of PLT, emphasizing its role in strengthening neural connections and promoting binocular integration.[5]
Given the promising results observed with PLT, this study aims to evaluate the long-term outcomes of amblyopic patients treated with PLT over a 5-year follow-up period. The investigation focuses on assessing visual acuity improvements, binocular function restoration, and the sustainability of therapeutic effects. By addressing the limitations of conventional treatments, this study seeks to establish PLT as a viable and effective approach for managing amblyopia.
MATERIAL AND METHODS
This prospective observational study was conducted at a tertiary eye care center in accordance with the tenets of the Declaration of Helsinki, with appropriate informed consent obtained from all participants. Subjects were recruited after achieving maximum visual improvement through optical correction and patching. A total of 89 individuals were enrolled in the study. Exclusion criteria included the presence of any ocular condition or cause of reduced visual acuity other than refractive errors, strabismus, or cataracts. The training sessions were structured to include 30–40 sessions, aligning with the manufacturer’s recommended minimum exposure. Each participant underwent three training sessions per week. The training was conducted using the best-corrected glasses. Anisometropic participants with a refractive difference of 3.5 diopters or more were prescribed contact lenses and instructed to wear them throughout the treatment period.
Revital Vision therapy employs a personalized, software-based approach to perceptual learning, focusing on visual stimulation. This therapy enhances neural connections through computer-based visual training, thereby improving visual acuity and contrast sensitivity in children with amblyopia. The software customizes treatment based on an individual’s performance during two calibration sessions, adapting to their responses and creating tailored treatment algorithms. Visual perception tasks were administered using a workstation (personal computer). The first session took place in the clinic under supervision, whereas subsequent sessions were conducted at home. The stimuli, known as Gabor patches, consisted of gray-level gratings with spatial frequencies ranging from 1.5 to 12.0 cycles per degree on a background luminance of 40 cdm−2. The monitor screen sizes used ranged from 15 to 26 inches, positioned at a viewing distance of 1.5 m, subtending an angle of 9° by 12°. Sessions were carried out in dark rooms, with the display screen serving as the sole light source.
Participants were presented with visual perceptual tasks displayed on a computer monitor and instructed to make selections between two forced-choice alternatives using a two-button mouse. During each task, participants viewed two brief displays of Gabor patches, either with or without high-contrast flanking collinear patches, presented in random order for durations ranging from 80 to 320 ms, with 500-ms intervals between displays. They were required to identify the display containing three Gabor patches, compared to the alternative without stimuli. Both eyes remained open during the tasks, and auditory feedback was provided for incorrect responses. Tasks followed a staircase method, progressing one step up and three steps down until the participant reached their visual threshold.
Throughout the training sessions, the spatial frequency and orientation of the stimuli were systematically adjusted. Sessions began with lower spatial frequencies, progressing to higher frequencies with varying orientations. Thresholds for the contrast-detection task were assessed using a one-up/three-down staircase method with increments of 0.1 log units to estimate stimulus strength at 79% accuracy. Following each session, results were automatically transmitted to the Company Data Center for analysis using a proprietary algorithm. At the end of the complete training regimen, visual acuity assessments were repeated and documented.
RESULTS
Demographics
A total of 89 patients were included in this study, with 48 (53.9%) being male. The mean age of the participants was 15.8 years. The distribution of subjects across age groups showed that 25 patients (28.1%) were <10 years old, 44 patients (49.4%) were between 11 and 20 years, 15 patients (16.9%) were between 21 and 30 years, and 5 patients (5.6%) were aged 31–40 years.
Amblyopia types
The most common type of amblyopia identified in this study was refractive amblyopia, accounting for 80 patients (89.87%). Deprivation amblyopia was observed in 2 patients (2.25%), whereas 4 patients (4.49%) had strabismic amblyopia. In addition, 3 patients (3.37%) had amblyopia caused by a combined mechanism.
Visual acuity
Visual acuity was evaluated at multiple time points, from baseline to the 5-year follow-up. The results demonstrated a statistically significant improvement in visual acuity between baseline and 1-year, 2-year, and 3-year visits [Table 1]. However, no statistically significant difference was observed between 1-year and 2-year visits, 1-year and 3-year visits, or visits beyond 3 years. At baseline, 109 eyes from 89 patients were assessed. Due to follow-up losses, the number of eyes reviewed decreased to 49 at 2 years, 26 at 3 years, and 24 at visits beyond 3 years. The mean LogMAR visual acuity improved from 0.56 ± 0.27 at presentation to 0.42 ± 0.26 at 1 year, 0.36 ± 0.26 at 1–2 years, 0.32 ± 0.24 at 2–3 years, and 0.30 ± 0.24 beyond 3 years. These results indicate a gradual improvement in visual acuity over time [Figure 1a and b].
| Pair | Difference | F statistic | P-value |
|---|---|---|---|
| Baseline – 1 year | 0.1 | 15.33 | 0.0006 |
| Baseline – (1–2) year | 0.13 | 16.40 | 0.0004 |
| Baseline – (2–3) year | 0.18 | 19.45 | 0.0002 |
| Baseline – (>3) year | 0.31 | 42.21 | <0.001 |
| 1 year – (1–2) year | 0.03 | 4.404 | 0.047 |
| 1 year – (2–3) year | 0.08 | 9.427 | 0.005 |
| 1 year – (>3) year | 0.21 | 33.48 | <0.001 |
| (1–2) year – (2–3) year | 0.05 | 7.219 | <0.001 |
| (1–2) year – (>3) year | 0.17 | 42.88 | <0.001 |
| (2–3) year – (>3) year | 0.12 | 40.38 | <0.001 |
F statistics are the values of F test
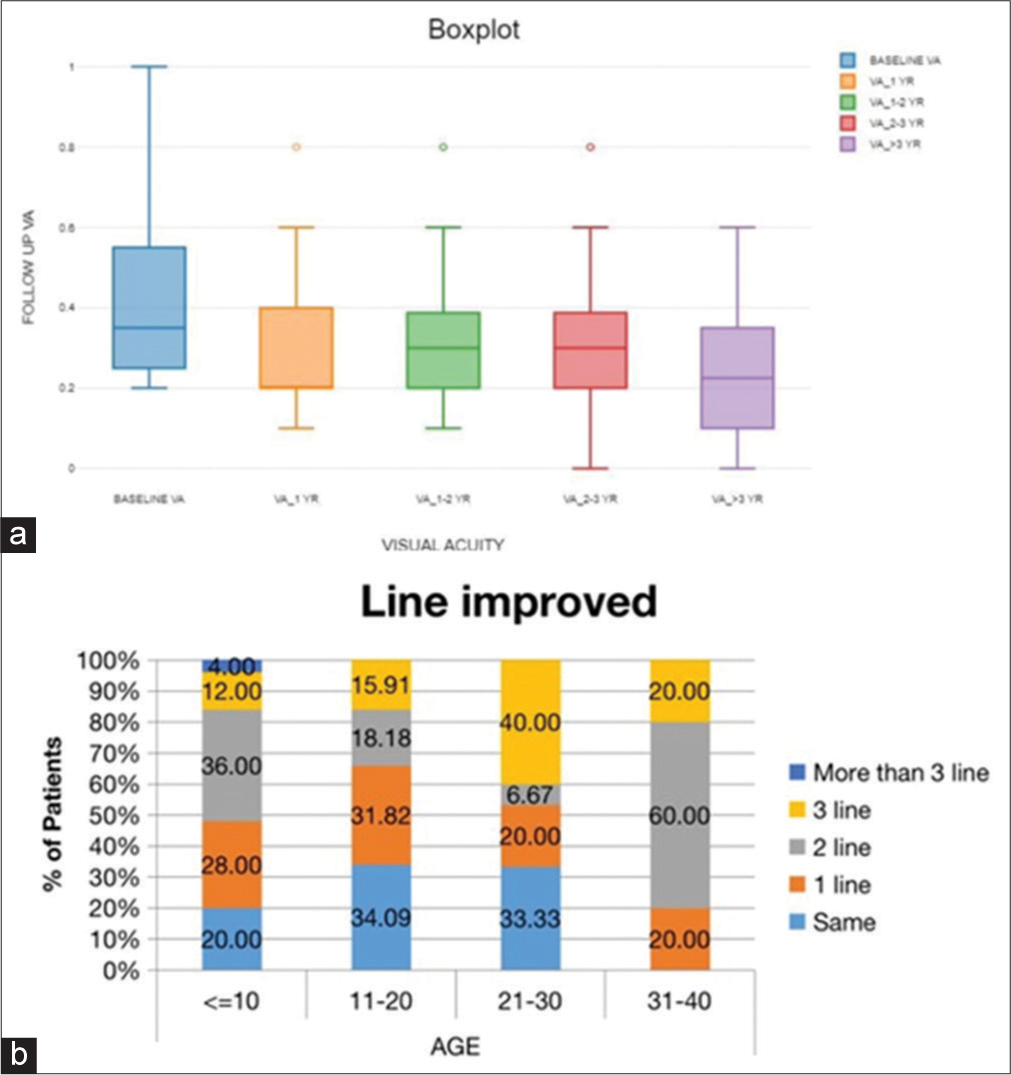
- (a) The box plot above demonstrates the visual acuity improvements from baseline and with each follow-up visit till the last review at 5 years. (b) Stacked bar chart shows the percentage of subjects with visual acuity improvement within the age group.
Visual acuity improvement versus age
The visual acuity improvements were analyzed based on age groupings, which included 25 subjects under 10 years, 44 subjects between 11 and 20 years, 15 subjects between 21 and 30 years, and 5 subjects between 31 and 40 years. Among these, 25 subjects showed a one-line improvement in visual acuity, 21 subjects showed a two-line improvement, and 17 subjects showed a three-line improvement. Only one subject, under the age of 10 years, achieved more than a three-line improvement. A total of 25 subjects showed no improvement in visual acuity after therapy; however, there was no deterioration in visual acuity in any subject [Table 2].
| Line Improvement | Age | Total | |||
|---|---|---|---|---|---|
| ≤10 | 11–20 | 21–30 | 31–40 | ||
| Same | 5 (20) | 15 (34.09) | 5 (33.33) | 0 (0) | 25 (28.09) |
| 1 line | 7 (28) | 14 (31.82) | 3 (20) | 1 (20) | 25 (28.09) |
| 2 lines | 9 (36) | 8 (18.18) | 1 (6.67) | 3 (60) | 21 (23.6) |
| 3 lines | 3 (12) | 7 (15.91) | 6 (40) | 1 (20) | 17 (19.1) |
| More than 3 lines | 1 (4) | 0 (0) | 0 (0) | 0 (0) | 1 (1.12) |
| Total | 25 (100) | 44 (100) | 15 (100) | 5 (100) | 89 (100) |
5-year change in bilateral amblyopia
Statistical analysis for bilateral amblyopia revealed a significant improvement in visual acuity across the five follow-up visits. The P = 0.001 indicated that the observed differences were unlikely to have occurred by chance, with a Type I error probability of only 0.19%. The test statistic (χ2) of 17.02 was outside the acceptance range (0, 9.48), and the effect size (W) of 0.53 suggested a large difference in ranks, confirming meaningful visual acuity improvement in patients with bilateral amblyopia.
5-year change in unilateral amblyopia
For unilateral amblyopia, statistical analysis also indicated significant improvement in visual acuity over the five follow-up visits. The P = 0.0002 suggested a very low probability (0.024%) of a Type I error. The test statistic (χ2) of 21.61 was outside the 95% acceptance region (0, 9.48), and the effect size (W) of 0.36 indicated a medium difference in ranks. These results demonstrate sustained improvement in visual acuity for patients with unilateral amblyopia over the 5-year follow-up period.
DISCUSSION
This study examined the long-term visual outcomes of amblyopia treatment over 5 years, focusing on visual acuity improvements and differences across amblyopia types and age groups. The results revealed significant improvements in visual acuity among participants, particularly in younger age groups and those with refractive amblyopia. Both unilateral and bilateral amblyopia showed meaningful gains, supporting the effectiveness of perceptual learning-based therapies combined with traditional treatments such as occlusion and optical correction.
The observed improvements in visual acuity align with findings from prior studies investigating perceptual learning and vision therapy in amblyopia management. Magdalene et al. demonstrated that neural vision perceptual learning resulted in significant visual improvements in amblyopic patients, highlighting the efficacy of targeted vision therapy programs.[5] Similarly, Tan and Fong reported that neural vision therapy enhances contrast sensitivity and visual acuity, particularly in low myopia cases, further validating the role of perceptual learning approaches in visual rehabilitation.[6]
In terms of long-term efficacy, our findings are consistent with studies by Milla et al., which emphasized the benefits of combining active vision therapy and occlusion in children with strabismic and anisometropic amblyopia.[7] Their work suggested that sustained improvements over several years could be achieved through structured therapy programs. The present study corroborates these results, particularly regarding gradual improvements over 5 years.
Younger participants showed greater visual acuity enhancements, consistent with Birch’s findings that younger age groups exhibit higher neuroplasticity, allowing more substantial visual recovery.[8] Our results revealed that children under 10 years achieved more than a three-line improvement, supporting prior evidence that early intervention yields better outcomes. Bankó et al. similarly reported that factors such as fixation instability and stereopsis limitations can impede recovery in older individuals, highlighting the importance of age-dependent variations in treatment responses.[9] However, improvements were not restricted to younger subjects. Older age groups also demonstrated measurable gains, consistent with research by Tsaousis et al., which emphasized the role of perceptual learning in promoting neural plasticity even in older amblyopic patients.[10] This highlights the adaptability of perceptual learning therapies across different age ranges, making them a viable option for older patients.
The statistically significant improvements observed in both bilateral and unilateral amblyopia groups suggest that treatment modalities were effective across varying severity levels. Studies by Thompson et al. emphasized harnessing brain plasticity to enhance binocular vision in amblyopia, aligning with our findings of sustained improvement over time.[11] Furthermore, Jin et al. highlighted the efficacy of binocular treatments compared to patching, supporting our results that visual gains can be achieved through therapies targeting neural mechanisms rather than solely relying on traditional occlusion methods.[12] In unilateral amblyopia, Li et al. demonstrated perceptual learning as a promising adjunct to occlusion therapy, showing enhancements in visual acuity similar to those observed in this study.[13] In addition, Jeter et al. confirmed that increased training specificity leads to greater visual gains, reinforcing the importance of structured therapy programs.[14]
The visual improvements in this study can be attributed to the neural mechanisms underlying perceptual learning, which enhance cortical processing and improve contrast sensitivity.[6] Studies have shown that perceptual learning targets visual pathways associated with amblyopic deficits, facilitating neural reorganization and improving visual performance.[4,15] Bankó et al. suggested that visual plasticity plays a critical role in visual recovery by addressing binocular imbalance and fixation instability.[9] This aligns with the present study’s findings, as significant improvements were noted even in older patients, indicating ongoing neural adaptability beyond the critical period.
Despite promising results, this study has several limitations. The sample size, though adequate for statistical analysis, limits broader generalization. Future studies should involve larger, multicenter cohorts to validate these findings. In addition, follow-up losses over 5 years may have introduced selection bias, as participants who discontinued therapy may have experienced less improvement.
The reliance on visual acuity as the primary outcome measure also poses limitations. Hess emphasized that visual acuity alone may not capture improvements in binocular vision, contrast sensitivity, or quality of life.[16] Future studies should incorporate measures of binocular function, stereopsis, and patient-reported outcomes to provide a more comprehensive assessment of treatment efficacy. Another limitation is the potential variability in adherence to therapy protocols. Searle et al. highlighted that compliance remains a significant factor influencing treatment outcomes, particularly in younger children.[17] Addressing compliance through parental counseling and behavioral interventions may optimize future results.
Future research should focus on integrating advanced technologies, such as virtual reality-based perceptual learning systems, to enhance patient engagement and compliance. Zhu et al. demonstrated promising outcomes using eye-tracking-based therapies, suggesting their potential as scalable alternatives to traditional methods.[18] In addition, investigations into biomarkers for treatment responsiveness, such as functional magnetic resonance imaging studies, may help identify patients likely to benefit from specific therapies.[19] Expanding treatment protocols to include combination therapies targeting binocular vision and neural plasticity could further optimize visual outcomes.[11] Studies evaluating long-term maintenance of visual gains post-therapy are also warranted. Hernández-Rodríguez et al. emphasized the importance of follow-up assessments to ensure sustained improvements and identify cases requiring additional interventions.[20]
CONCLUSION
This study highlights the long-term efficacy of amblyopia treatments, demonstrating significant visual acuity improvements across different age groups and amblyopia types. The findings reinforce the role of perceptual learning-based therapies in promoting neural plasticity and visual rehabilitation. While younger patients showed greater improvements, older age groups also benefited, supporting the adaptability of these therapies. However, limitations related to sample size, follow-up attrition, and reliance on visual acuity metrics must be addressed in future research. Integrating advanced technologies and combination therapies could further enhance treatment efficacy, ensuring sustained improvements in visual function.
Ethical approval
The research/study was approved by the Institutional Review Board at Sri Sankaradeva Nethralaya, number 26, dated 6th May 2017.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Amblyopia: Prevalence, natural history, functional effects and treatment. Clin Exp Optom. 2005;88:365-75.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of vision-based treatments for children and teens with amblyopia: A systematic review and meta-analysis of randomised controlled trials. BMJ Open Ophthalmol. 2021;6:e000657.
- [CrossRef] [PubMed] [Google Scholar]
- Perceptual learning as a potential treatment for amblyopia: A mini-review. Vis Res. 2009;49:2535-49.
- [CrossRef] [PubMed] [Google Scholar]
- Neural vision perceptual learning as an effective treatment of amblyopia. Vision Dev Rehab. 2022;8:260-9.
- [CrossRef] [Google Scholar]
- Efficacy of neural vision therapy to enhance contrast sensitivity function and visual acuity in low myopia. J Cataract Refract Surg. 2008;34:570-7.
- [CrossRef] [PubMed] [Google Scholar]
- Combined treatment of active vision therapy and occlusion in children with strabismic and anisometropic amblyopia: A 5-year follow-up. J Pediatr Ophthalmol Strabismus. 2013;50:222-8.
- [Google Scholar]
- Amblyopia and binocular vision. Prog Retin Eye Res. 2013;33:67-84.
- [CrossRef] [PubMed] [Google Scholar]
- Amblyopic deficits in the timing and strength of visual cortical responses to faces. Cortex. 2013;49:869-81.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of perceptual learning-based vision therapy in adult amblyopes: A meta-analysis. Clin Exp Ophthalmol. 2014;42:642-51.
- [Google Scholar]
- Brain plasticity in the adult: modulation of function in amblyopia with rTMS. Curr Biol. 2008;18:1067-71.
- [CrossRef] [PubMed] [Google Scholar]
- Patching and suppression in amblyopia: Learning from the failure of the binocular approach. Vis Res. 2011;51:980-90.
- [Google Scholar]
- Video-game play induces plasticity in the visual system of adults with amblyopia. PLoS Biol. 2011;9:e1001135.
- [CrossRef] [PubMed] [Google Scholar]
- Task precision at transfer determines specificity of perceptual learning. J Vis. 2009;9:1-13.
- [CrossRef] [PubMed] [Google Scholar]
- Making perceptual learning practical to improve visual functions. Vis Res. 2009;49:2566-73.
- [CrossRef] [PubMed] [Google Scholar]
- Compliance with occlusion therapy for amblyopia: A pilot study. Psychol Health Med. 2002;7:529-36.
- [Google Scholar]
- Interocular transfer of perceptual learning in amblyopia. Invest Ophthalmol Vis Sci. 2013;54:455-63.
- [Google Scholar]
- Prentice award lecture 2011: Removing the brakes on plasticity in the amblyopic brain. Optom Vis Sci. 2012;89:827-38.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of amblyopia treatment in children aged 7 to 12 years. J AAPOS. 2014;18:453-6.
- [Google Scholar]






