Translate this page into:
Case report: Application of prosthetic soft contact lens as bandage contact lens for band keratopathy

*Corresponding author: Sona Paul, Department of Contact Lens, Medical Research Foundation, Sankara Nethralaya, Chennai, Tamil Nadu, India. sonapaul699@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Paul S, Iqbal A. Case report: Application of prosthetic soft contact lens as bandage contact lens for band keratopathy. Lat Am J Ophthalmol 2023:6:15.
Abstract
Soft prosthetic contact lenses (PCL) offer the broadest cosmetic options to enhance the appearance of sighted, non-sighted diseased or disfigured eyes. A forty-six-year-old female with a previous history of injury to the right eye with a pencil, presented to contact lens clinic with complaints of irritation, discomfort, and sensitivity to bright light. The patient was advised to use antibiotics and lubricants along with BCL to improve comfort. Initially, BCL was recommended as continuous wear to improve the comfort level. During the follow-up visit, the patient was concerned about cosmesis and symptom relief at the same time. The patient was fitted with type D prosthetic soft contact lens with continuous wear. This case report highlights the dual use of PCL. It enhances the cosmesis acts as a therapeutic agent or BCL.
Keywords
Soft prosthetic contact lenses
Bandage contact lenses
Photorefractive keratectomy
Phototherapeutic keratectomy
Corneal collagen cross-linking
INTRODUCTION
Prosthesis means restoring a disfigured or missing part of the body and improving the appearance. Soft prosthetic contact lenses (PCLs) offer the broadest cosmetic options to enhance the appearance of sighted or non-sighted diseased or disfigured eyes. PCLs are easier to fit in a wider range of corneal diseases, with excellent cosmesis, comfort, and overall outcome. PCL includes an occluded pupil with a clear iris, a tinted iris with no defined pupil, a tinted iris with a clear pupil, and a tinted iris with an occluded pupil. These have been previously described as Type A, B, C, and D.[1] The commercially available broader range of colors, designs, powers, and lens materials, along with advanced manufacturing and customization options allow the practitioner to design a contact lens that closely matches the patient’s natural eye color and normalizes the appearance.[2]
Bandage contact lenses (BCLs) can be used in an underlying disease state or to protect the cornea from the environment or mechanical interaction with the lid, treat ocular discomfort, and support the cornea during healing after surgery.[3] It is also incorporated into surface ablation procedures such as photorefractive keratectomy, laser-assisted in situ keratomileusis, phototherapeutic keratectomy (PTK), and corneal collagen cross-linking, to attenuate post-operative pain and reduces the need for topical and/or systemic analgesia.[3] It again protects the regenerating epithelium from shear stress induced by blinking and promotes re-epithelialization.[3,4]
A variety of contact lenses from high water content hydrogel lens to high oxygen permeable silicone hydrogel contact lenses can be utilized to accomplish the goal. BCLs can be used as a daily or extended wear modality depending on the ocular condition.[4] Along with external insult, the BCLs act as a comfort cushion and reduce the shear force created between lids and ocular surfaces during the blink. Worldwide there are a variety of BCLs available which covers a wider range of materials with different oxygen permeability, diameters, base curves, power, and modality.[3,4]
Band-shaped keratopathy (BSK) is a corneal degeneration, caused by chronic inflammation, and systemic abnormalities, characterized by calcium hydroxyapatite deposition in Bowman’s layer.[5] These deposits range from grayish-tochalky white in color with the progression of degeneration. As the disease progresses the calcium depositions can extend anteriorly and if it erodes through the epithelium can cause foreign body sensation, irritation, and persistent epithelial defect. BCL, along with concomitant antimicrobial topical therapy plays an important, effective, and considerable role in the eyes with BSK.[6] The most important indication is to prevent the mechanical interaction between the palpebral conjunctiva and elevated calcium depositions in the cornea to reduce the patient symptoms while blinking. Patients with major concerns about cosmesis can be fitted with a prosthetic contact lens to enhance their appearance.
This case report enlightens the dual use of a prosthetic soft contact lens. It enhanced the cosmesis as well as acted as a therapeutic or BCL.
CASE REPORT
A 46–year–old female presented to our contact lens clinic on January 2021 with complaints of irritation and discomfort in her right eye. Her past ocular history revealed that she underwent multiple ocular surgeries which include corneal tear repair, lensectomy, membranectomy, and anterior vitrectomy for the same eye. The patient was occasional spectacle wear for distance vision and near vision. The patient’s medical and family history were negative, and she denied taking any medications or having allergies to the same. The patient reports no history of migraines and her blood pressure was within normal limits. The best-corrected visual acuity in the right eye was no perception of light and the left eye 20/20 with −2.25 DS and N6 with near addition of +1.50 DS. Pinhole acuity at a distance was showing no improvement. Anterior segment evaluation by slit lamp shows both eyes were within normal limits with a quiet bulbar and palpebral conjunctiva with clear lashes. Left eye intact clear cornea, irises were brown, anterior chamber appeared clear without cells or flare and the estimate of the anterior chamber angles was 4/4 by Van Herrick. The right eye shows ciliary staphyloma with BSK with corneal vascularization [Figure 1a]. Because of no further surgical intervention, the patient was advised to use antibiotics (Vigamox eye drop) and lubrication eye drops (refresh tears) along with BCL to give her better comfort. Initially, BCL was recommended for continuous use to prevent mechanical interaction and to improve the comfort level. She was fitted with an AIR OPTIX AQUA by Alcon (Lotrafilcon B, 33% water content) BCL with an 8.6 mm base curve −0.50DS power and 14.2 mm diameter in her right eye. The patient was advised to change the lens after every 1 month of continuous use.
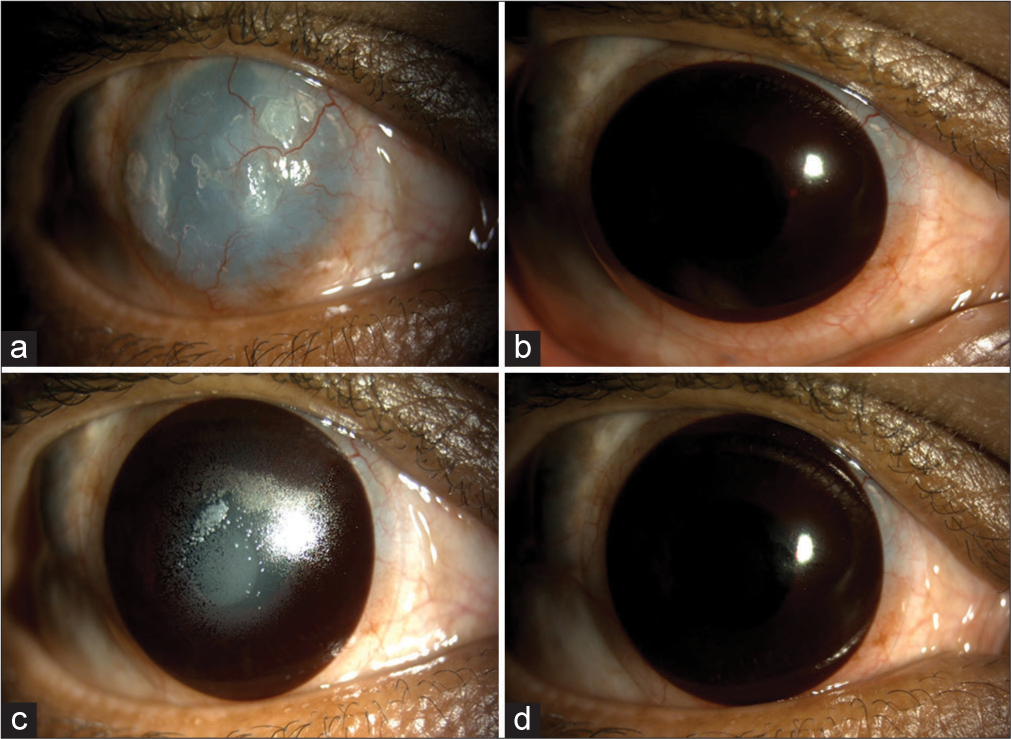
- (a) Band-shaped keratopathy with corneal vascularization with calcium, (b) Type D soft prosthetic contact lenses (PCL), (c) Dense lens deposits, (d) New prosthetic Type D PCL.
Follow-up # 1
During review visits to the contact lens clinic, the patient reported improved comfort and reduced symptoms with BCL on the eye but the patient was concerned about cosmesis and also needed to maintain the symptomatic relief at the same time. After discussing the possible and available lens options, a soft prosthetic contact lens was suggested as both a cosmetic lens and BCL, which will improve cosmetic appearance and symptomatic relief at the same time. The patient was fitted with a Silver line Type D (tinted iris with an occluded pupil) prosthetic soft contact lens (25% Poly 2 hydroxyethyl methacrylate, 75% water content) with a base curve of 8.60 mm and diameter of 14.00 mm. She was fitted with a dark brown iris tint which was matching the iris color of the fellow eye and was giving a better cosmetic appearance [Figure 1b]. The patient was very much happy with cosmesis and reported a significant reduction in symptoms.
Follow-up # 2
The patient again visited the clinic after 1 week, and reported a significant improvement in comfort level, no difficulty with bright light, and improved quality of life. She was instructed to wear the lens for a continuous 30 days and then to give a gap of 1 day and to insert a new lens. Although she was advised a monthly review in the contact lens clinic for lens exchange, the lens insertion, removal, and cleaning techniques were taught to her in case of any emergency need. She was advised to continue her habitual spectacle corrections over the contact lens.
Follow-up # 3
After 6 months, she reported to the clinic with complaints of irritation and discomfort and a feeling of excessive lens movement. Slit-lamp examination showed dense deposits of the lens surface [Figure 1c]. During history taking, the patient reported over usage of the prescribed contact lens for almost more than 2 months as she was not able to report to the clinic and was out of stock of lens due to the pandemic. The old lens was discarded and the patient was fitted with a new lens with the same parameters [Figure 1d]. As long as the patient did not experience any issues with her contact lens, she was counseled to return in every 6 months for a comprehensive annual examination and detailed contact lens examination.
DISCUSSION
BCLs act as a shield from external factors reduces mechanical friction and promote hydration and protection to the compromised ocular surface. Any contact lens which protects the eye, enhance comfort, facilitate healing, and sealing wound leak is considered a therapeutic BCLs.[4] High oxygen transmissible silicone hydrogel lenses are considered a preferable option due to their better bandage effect and reduced hypoxia-related effects on extended wear.[4]
PCLs are mainly indicated in disfigured eyes to hide the defect or abnormality, enhance the appearance, and reducing visual symptoms.[7,8] The silicone hydrogel PCLs are not available with Indian manufacturers and hence the patient in this report was fitted with a high water content hydrogel material to improve the oxygen permeability to some extent. Due to its material characteristics, these lenses are advised to be used as a conventional modality with daily wear and as a frequent replacement modality when advised to be used as continuous wear.
The natural history of band keratopathy is a gradual progression over many months/years; in most cases it is superficial.[6] In the early stages of the condition, the patients remain asymptomatic; however, extension into the visual axis can result in glare and reduced visual acuity.
There are different treatment options available to remove band keratopathy, such as mechanical debridement, use of ethylene-diamine-tetra-acetic acid in isolation, or supplemented with superficial keratectomy (manual or excimer laser PTK) or amniotic membrane transplant.[9,10] The patient did not undergo any such treatment as it was in the early to moderate stage of the disease and she was able to manage with a prosthetic contact lens.
In this case, the calcium deposits were extending anteriorly and were causing irritation discomfort, and difficulties in bright light, and the patient also raised a concern about the cosmesis. The transparent AIR OPTIX AQUA BCL was taking care of her comfort level but failed to provide her with better cosmesis and reduced bright light issues. Whereas a prosthetic Type D lens with dark brown iris tint was taking care of the symptoms and enhancing the cosmetic appearance and a better quality of life. A regular follow-up with in-clinic BCL change is recommended to avoid any complications.
CONCLUSION
PCLs can be utilized as a therapeutic or BCLs and, at the same time, can be beneficial to mask the disfigurement and give a better appearance. The practitioners should be aware of the dual use of PCL while handling a patient with a disfigured eye requires fitting BCLs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Soft prosthetic contact lens practice in Indian scenario. Asian J Ophthalmol. 2017;15:22.
- [CrossRef] [Google Scholar]
- Use of soft contact lens for esthetic and functional rehabilitation. Eye Contact Lens. 2021;47:383-7.
- [CrossRef] [PubMed] [Google Scholar]
- BCLA CLEAR-medical use of contact lenses. Contact Lens Anterior Eye. 2021;44:289-329.
- [CrossRef] [PubMed] [Google Scholar]
- Application of senofilcon a contact lenses for therapeutic bandage lens indications. Eye Contact Lens. 2013;39:315-23.
- [CrossRef] [PubMed] [Google Scholar]
- Acute calcific band keratopathy: Case report and literature review. J Cataract Refract Surg. 2013;39:292-4.
- [CrossRef] [PubMed] [Google Scholar]
- Band keratopathy in children previously treated with diode laser for Type 1 retinopathy of prematurity. J AAPOS. 2019;23:232-4.
- [CrossRef] [PubMed] [Google Scholar]
- Managing visual symptoms in cone-rod dystrophy with prosthetic soft contact lens: A case report. Indian J Ophthalmol Case Rep. 2023;3:86.
- [CrossRef] [Google Scholar]
- Masking the red reflex of flash photography with prosthetic lenses. Eye Contact Lens. 2022;48:537-9.
- [CrossRef] [PubMed] [Google Scholar]
- New treatment for band keratopathy: Superficial lamellar keratectomy, EDTA chelation and amniotic membrane transplantation. J Korean Med Sci. 2004;19:611-5.
- [CrossRef] [PubMed] [Google Scholar]
- Management of band keratopathy with excimer phototherapeutic keratectomy. Eye (Lond). 2006;20:252.
- [CrossRef] [PubMed] [Google Scholar]







