Translate this page into:
Incidence and clinical profile of Marcus Gunn jaw-winking phenomenon in congenital ptosis at a tertiary eye hospital in western Uttar Pradesh, India

*Corresponding author: Suraj Kumar Chaurasiya, Department of Optometry and Vision Science, CL Gupta Eye Institute, Moradabad, Uttar Pradesh, India. csurajk414@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chaurasiya SK, Alam MM, Agarwal P, Chauhan L. Incidence and clinical profile of Marcus Gunn jaw-winking phenomenon in congenital ptosis at a tertiary eye hospital in western Uttar Pradesh, India. Lat Am J Ophthalmol 2023:6:4.
Abstract
Objectives:
The objectives of this study were to report the hospital-based incidence and a rare case series of Marcus Gunn jaw-winking phenomenon (MGJWP) in patients with congenital ptosis
Material and Methods:
This was a retrospective non-interventional case series. The medical records of all patients diagnosed with MGJWP over the past 3.5 years were retrieved from the electronic medical record. Patients with documented evidence of the presence of ptosis with MGJWP were included and analyzed for visual acuity, the presence of squint and amblyopia, and the presence of other aberrant regenerations.
Results:
A total of 198 patients were diagnosed with congenital ptosis, out of which 23 (11.6%) patients had MGJWP along with congenital ptosis and 175 (84.4%) patients have congenital ptosis without MGJWP. There were 12 males and 11 females. The mean age at presentation was 10.35 ± 8.4 years (range from 2 to 28 years). All the patients presented unilateral MGJWP. The right eye was involved in seven patients (30.4%) and the left eye in 16 patients (69.5%). Most of the patients had observed the onset of MGJWP by parents since birth. Visual acuity was measured by Snellen’s distance acuity chart in 15 patients. Eight patients were preverbal, and their vision was assessed by the fixation pattern, which was central, steady, and maintained. Nine patients (39.1%) were emmetropic, seven patients (30.4%) had astigmatism, and seven patients were amblyopic in the affected eye. Strabismus was noted in nine patients (39.1%) in this study. Monocular elevation deficiency was noted in five patients, three patients have exotropia, and one had hypotropia.
Conclusion:
All the patients had a mild form of MGJWP with no intervention required in any of the cases. The hospital-based incidence of MGJWP in congenital ptosis is 11.6%. Most of the patients had observed the onset of MGJWP by their parents since birth.
Keywords
Marcus Gunn jaw-winking phenomenon
Congenital ptosis
Incidence
INTRODUCTION
Marcus Gunn jaw winking phenomenon (MGJWP) is an unusual condition that is present at birth.[1] This was first described by Robert Marcus Gunn in 1883 and is also known as the Marcus Gunn jaw-winking phenomenon.[2] It is characterized by involuntary movement of the upper eyelid in a rapid rising motion each time the jaw moves.[1] The wink phenomenon may be triggered by various movements of the mandible.[3] Other ocular abnormalities and vision problems may also occur.[2] It usually affects one eye but it can affect both eyes also in rare cases.[3] The exact cause of this phenomenon is not yet understood. Marcus Gunn jaw winking phenomenon is generally unpredictable, but familial cases have been reported.[3,4] The treatment is not always needed but may include surgery in more severe cases.[1]
This condition is found in approximately 2–13% of all cases of congenital ptosis.[5] The purpose of this study was to report the incidence of associated MRJWP in a series of patients with congenital ptosis.
MATERIAL AND METHODS
This was a retrospective non-intervention case series. The study has been reviewed and approved by Institutional Review Board and was conducted in compliance with Declaration of Helsinki. All the data related to was reviewed from the electric medical records over a period of 3.5 years from February 2017 to November 2020. MGJWP in congenital ptosis is defined as the presence of congenital ptosis and MGJWP in the affected eye. Demographic data included analysis of age at presentation, sex, and laterality. Clinical data analysis included refractive diagnosis, presence of squint and amblyopia, presence of aberrant regenerations, and extraocular motility. Data were analyzed using Microsoft Office Excel 2013.
RESULTS
A total of 198 patients were diagnosed with congenital ptosis, out of which 23 (11.6%) patients had MGJWP, along with congenital ptosis and 175 (88.4%) patients have congenital ptosis without MGJWP. Of 23, 12 were male and 11 females. The mean age at presentation was 10.35 ± 8.4 years (range 2–28 years). The median age was 8 years. All the patients presented unilateral MGJWP. The right eye was involved in seven patients (30.4%) and left eye in 16 patients (69.5%) [Table 1]. Most of the patients had observed the onset of MGJWP by parents since birth. All except four patients had been delivered at full term by normal delivery. Four patients were delivered by cesarean.
| Parameters | Number | % |
|---|---|---|
| Age (years) | 10.35±8.4 (range 2–28) | |
| Male: Female | 12:11 | |
| Right eye: Left eye | 7:16 | 30.4:69.5 |
| Total number of congenital ptosis | 198 | |
| Incidence of MGJWP in congenital ptosis | 23 | 11.6 |
| Total congenital ptosis without MGJWP | 175 | 88.4 |
Visual acuity was measured by Snellen’s distance acuity chart in fifteen patients. Eight patients were preverbal, and their vision was assessed by the fixation pattern, which was central, steady, and maintained. Nine patients (39.1%) were emmetropic, seven patients (30.4%) had astigmatism, and seven patients were amblyopic in the affected eye [Figure 1]. Strabismus was noted in nine patients (39.1%). Monocular elevation deficient was noted in five patients, three patients had exotropia, and one had hypotropia [Figure 2]. One patient underwent a ptosis surgery and one underwent squint surgery.
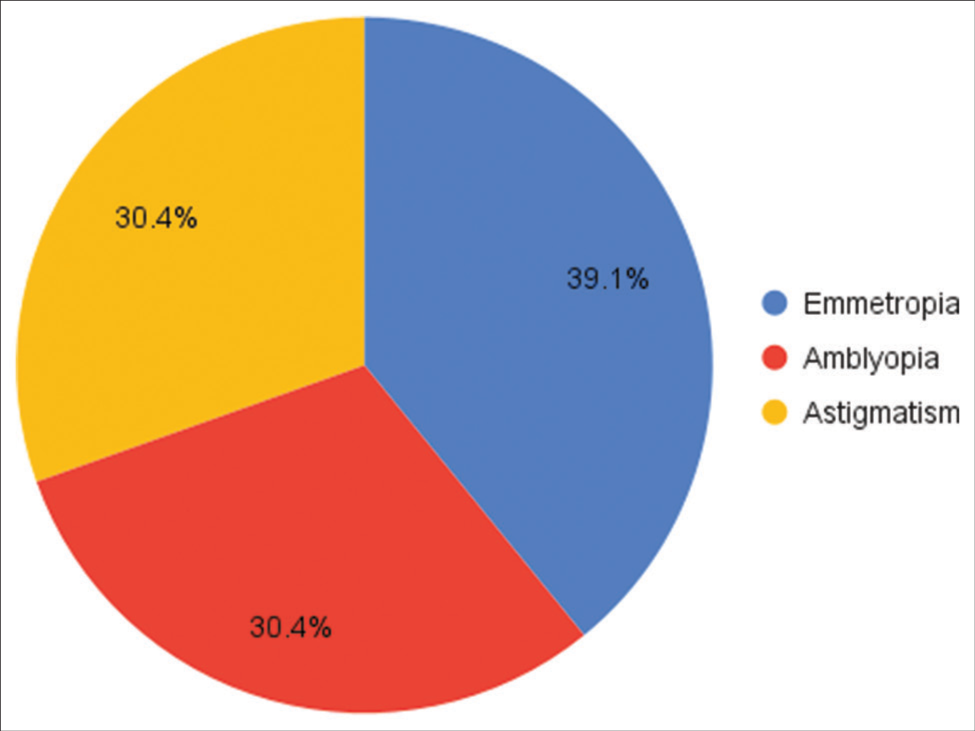
- Refractive error in Marcus Gunn jaw-winking phenomenon.

- Types of strabismus in Marcus Gunn jaw-winking phenomenon.
DISCUSSION
MGJWP is usually associated with a variable amount of ptosis that manifests at the same time as the synkinesis itself.[1,6] In this case series, 23 patients had MGJWP with congenital ptosis. One case of MGJWP without ptosis was reported by Pratt et al. in their review of 71 cases and this was the only case reported over the past 150 years until the case series of 72 patients reported by Pearce et al. recently.[5,6] Pearce et al. reported that 8.5% of the patients with MGJWP with congenital ptosis, we noticed 11.6% in our cohort.
All the patients in our series showed unilateral presentation. MGJWP usually presents unilaterally, but rarely can be seen bilaterally.[7-9] All 23 patients demonstrated typical upper eyelid elevation on chewing or sucking. Although lid elevation is commonly associated with chewing or sucking movements, it has been reported with other movements such as lateral mandibular movement, yawning, smiling, sternocleidomastoid contraction, tongue protrusion, Valsalva maneuver, or even during inspiration.[10-12] There were no dental anomalies associated with our subset of patients; however, there have been a few case reports that describe malocclusion, proclined upper anterior teeth, severe lower crowding, and mandibular micrognathia associated with MGJWP.[13,14]
There was no gender preponderance in our series of patients, which concurs with previous studies.[15] The left eye was more commonly affected (69.5%) in our study. Doucet et al. also reported a slight left eye preponderance in their series of MGJWP patients.[16] This has been attributed to fibrin emboli preferentially traveling to the left carotid vessels in utero due to the asymmetry of thoracic vasculature.[17] However, Demirci et al. found no statistically significant difference between eye involvement.[15]
All the patients of congenital MGJWP in our case series were born full term. No significant history of parental insult was documented that four patients had been delivered at full term by normal vaginal delivery, while four patients in our case series had been delivered by cesarean delivery.
Despite numerous case reports and a number of case series on MGJWP, the exact mechanism of this fascinating phenomenon is yet to be clearly understood. There are two schools of thought. The first one believes in the “release hypothesis,” according to which aberrant connections between appositionally adjacent trigeminal mesencephalic nucleus and the oculomotor nucleus are a part of primitive reflex which got extinguished during phylogenetic development. This primitive reflex gets released and becomes active due to intrauterine trauma or some unknown causes, resulting in the synkinetic lid and jaw movement.[18,19] Hiscock and Straznicky have proven that such a primitive reflex would have helped an amphibian focus on its prey even with its mouth open wide.[20] Lehman et al. went on to demonstrate the existence of this reflex in normal adults with trigeminal neuralgia, with the help of electromyography.[21]
The second hypothesis is that MGJWP is due to some structural abnormality in the brainstem which causes neural misdirection of trigeminal motor axons to levator palpebrae superioris (LPS).[22] Other theories are pre-existing aberrant connections and ephaptic transmission between the mandibular division of trigeminal nerve innervating the pterygoids and the superior division of oculomotor nerve innervating LPS.[12,23,24]
Retrospective design, no documentation of the type of jaw movement eliciting Marcus-Gunn, grading of ptosis, and short follow-up period for a few of the patients are some of the limitations of the present study.
CONCLUSION
All the patients had a mild form of MGJWP with no intervention required in any of the cases. The hospital-based incidence of MGJWP in congenital ptosis is 11.6%. Most of the patients had observed the onset of MGJWP by parents since birth.
Declaration of patient consent
The Institutional review board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- National Organization for Rare Disorders (NORD) 2003. Available from: https://www.rarediseases.org/rare-diseases/marcus-gunn-phenomenon [Last assessed on 2008 Mar 24]
- [Google Scholar]
- The Marcus Gunn phenomenon; discussion, presentation of four instances and consideration of its surgical correction. Am J Ophthalmol. 1947;30:143-58.
- [CrossRef] [PubMed] [Google Scholar]
- Marcus Gunn Jaw-winking Syndrome. 2015. Medscape Reference. Available from: https://www.emedicine.medscape.com/article/1213228-overview [Last assessed on 2023 Jan 24]
- [Google Scholar]
- Orphanet. 2007. Available from: https://www.orpha.net/consor/cgi-bin/oc_exp.php?lng=en&expert=91412 [Last assessed on 2007 Apr]
- [Google Scholar]
- The Marcus Gunn phenomenon. A review of 71 cases. Ophthalmology. 1984;91:27-30.
- [CrossRef] [PubMed] [Google Scholar]
- Marcus Gunn jaw-winking syndrome: A comprehensive review and report of four novel cases. Ophthalmic Plast Reconstr Surg. 2017;33:325-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Marcus Gunn jaw-winking syndrome. Neurology. 2015;84:1061.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral jaw winking reflex in association with multiple congenital anomalies. Arch Ophthalmol. 1960;64:946-9.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral Marcus Gunn jaw winking synkinesis with monocular elevation deficiency: A case report and literature review. Int Ophthalmol. 2012;32:199-201.
- [CrossRef] [PubMed] [Google Scholar]
- Marcus Gunn phenomenon: Differential diagnosis of palpebral ptoses in children. J Pediatr (Rio J). 2004;80:249-52.
- [CrossRef] [PubMed] [Google Scholar]
- Pterygoid-levator synkinesis: The Marcus Gunn jaw-winking phenomenon. J Neuroophthalmol. 1987;7:61-2.
- [Google Scholar]
- Normal and abnormal eyelid function In: Walsh and Hoyt's Clinical Neuro-Ophthalmology. Pennsylvania, United States: Lippincott Williams and Wilkins; 2005.
- [Google Scholar]
- Marcus Gunn (jaw-winking) phenomenon: A case report. Spec Care Dentist. 2009;29:138-40.
- [CrossRef] [PubMed] [Google Scholar]
- Jaw-winking phenomenon: Report of a case with review of literature. Indian J Dent Res. 2015;26:320-3.
- [CrossRef] [PubMed] [Google Scholar]
- Marcus Gunn jaw-winking synkinesis: Clinical features and management. Ophthalmology. 2010;117:1447-52.
- [CrossRef] [PubMed] [Google Scholar]
- The quantification, natural course, and surgical results in 57 eyes with Marcus Gunn (jaw-winking) syndrome. Am J Ophthalmol. 1981;92:702-7.
- [CrossRef] [PubMed] [Google Scholar]
- Thromboembolism and congenital malformations: From Duane syndrome to thalidomide embryopathy. JAMA Ophthalmol. 2013;131:439-47.
- [CrossRef] [PubMed] [Google Scholar]
- Winking-jaw phenomenon. Arch Neurol Psychiatry. 1948;59:734-53.
- [CrossRef] [PubMed] [Google Scholar]
- Peripheral and central terminations of axons of the mesencephalic trigeminal neurons in Xenopus. Neurosci Lett. 1982;32:235-40.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence of ancillary trigeminal innervation of levator palpebrae in the general population. J Clin Neurosci. 2014;21:301-4.
- [CrossRef] [PubMed] [Google Scholar]
- Kinematic and diffusion tensor imaging definition of familial Marcus Gunn jaw-winking synkinesis. PLoS One. 2012;7:e51749.
- [CrossRef] [PubMed] [Google Scholar]
- Ephaptic transmission between single nerve fibres in the spinal nerve roots of dystrophic mice. J Physiol. 1980;305:151-69.
- [CrossRef] [PubMed] [Google Scholar]
- Marcus Gunn jaw winking with trigemino-abducens synkinesis. J AAPOS. 2000;4:316-7.
- [CrossRef] [PubMed] [Google Scholar]






