Translate this page into:
Phacoemulsification in posterior polar cataracts with a soft nucleus: Simple as ABC with proper techniques and precautions

*Corresponding author: Balamurugan Ramatchandirane, Department of Ophthalmology, All India Institute of Medical Sciences, Guntur, Andhra Pradesh, India. bala16690@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Devalla MD, Prasad SS, Ramatchandirane B. Phacoemulsification in posterior polar cataracts with a soft nucleus: Simple as ABC with proper techniques and precautions. Lat Am J Ophthalmol. 2024;7:16. doi: 10.25259/LAJO_33_2024
Abstract
Posterior polar cataract (PPC) is a type of cataract characterized by opacification at the posterior pole of the lens. It poses unique challenges during surgical management due to its tendency for capsular weakness, which increases the risk of complications during phacoemulsification. If the nucleus is soft (grade <2), removal using phacoemulsification is easy after it has been delineated using hydrodelineation and viscodelineation. In this case, we aim to demonstrate and educate on the proper steps for performing phacoemulsification surgery under topical anesthesia for a 36-year-old woman who presented with PPC grade II (as per Daljit Singh classification) with a soft nucleus in her right eye.
Keywords
Posterior polar cataract
Phacoemulsification
PPC
Soft nucleus
Cataract surgery
INTRODUCTION
Posterior polar cataract (PPC) is a type of cataract characterized by opacification at the posterior pole of the lens.[1] It poses unique challenges during surgical management due to its tendency for capsular weakness, which increases the risk of complications during phacoemulsification. Various techniques[1-3] have been described for managing PPCs with nuclear sclerosis grades >2, including the trident technique, two-Y crushing technique, and lambda technique. However, if the nucleus is soft (grade <2),[1] removal using phacoemulsification is easy after it has been delineated using hydrodelineation and viscodelineation. In this case, we aim to demonstrate and educate on the proper steps for performing phacoemulsification surgery under topical anesthesia [Video 1] for a 36-year-old woman who presented with PPC grade II[2] (as per Daljit sing classification) with a soft nucleus in her right eye [Figure 1a].
Video 1:
Video 1:Illustrates the important surgical steps of the posterior polar cataract with soft nucleus.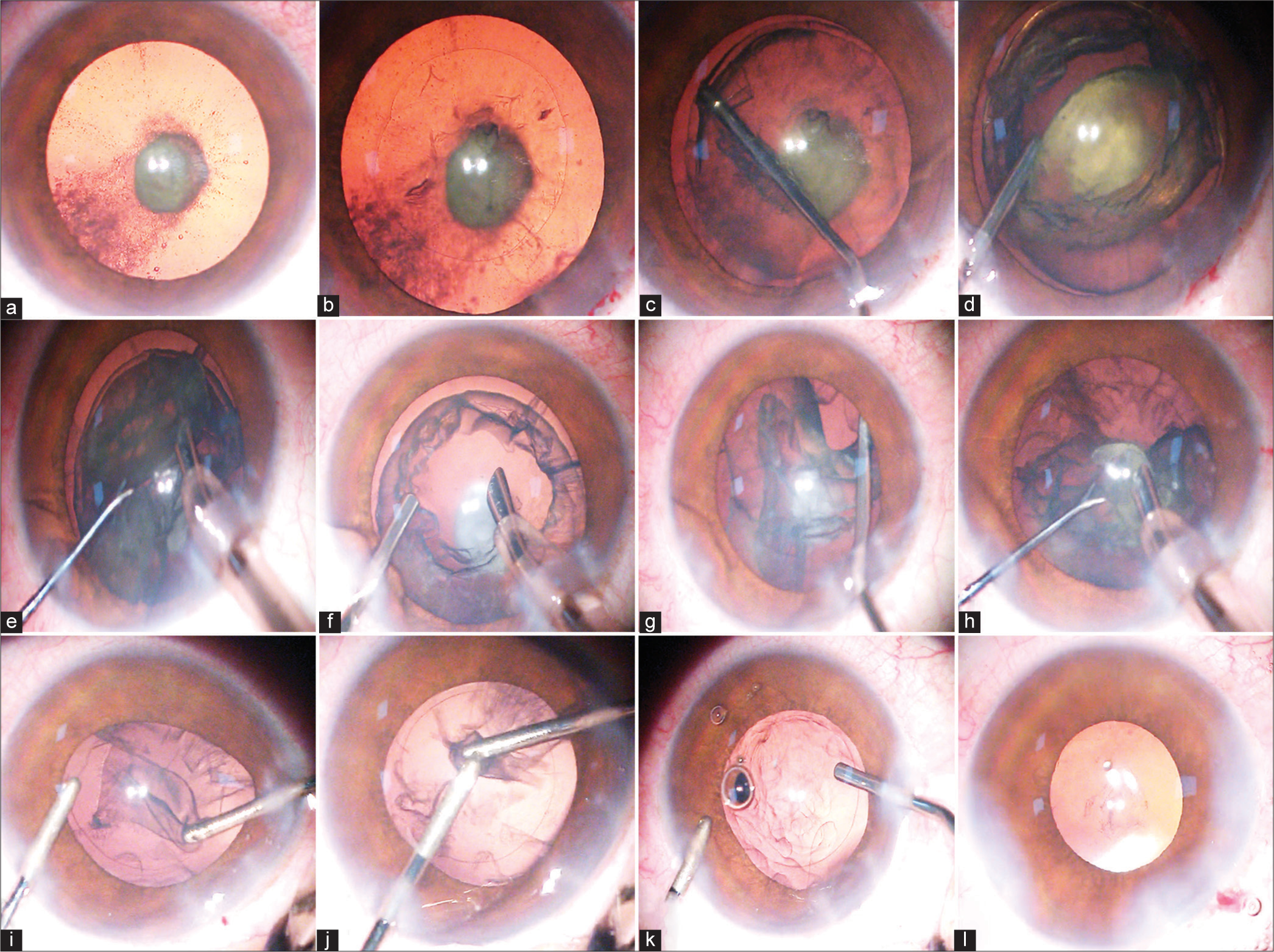
- (a) shows the posterior polar cataract grade II with a soft nucleus. (b) shows the approximate 5 mm continuous curvilinear capsulorhexis. (c) shows hydrodelineation. (d) shows the viscodelineation to prolapse the nucleus. (e) shows the emulsification of the soft nucleus using Tilt- and-crush technique. (f) shows the injection of hydroxypropyl methyl cellulose 2% to form the anterior chamber before the removal of the irrigation source (phaco probe). (g) shows the viscodissection to separate the epinucleus from the capsule. (h) shows the removal of the epinucleus using the phaco probe. (i) shows the mechanical removal of the cortex using the aspiration probe with less vacuum and crushing it with irrigation cannula. (j) crushing the cortical matter using bimanual irrigation and aspiration cannula followed by removal using low vacuum. (k) shows the injection of the viscoelastic before removal of the irrigation cannula (irrigation source). (l) shows the implantation of the single piece intraocular lens in the bag.
Key steps for phacoemulsification in PPC with soft cataracts
Phacoemulsification settings should remain low,[1] with ultrasound energy around 20, bottle height at approximately 70 mmHg, and vacuum levels between 150 and 200 mmHg.
Side Ports: Create side ports at the 10 and 2 o’clock positions using a 15-degree blade.
Viscoelastic Injection: Inject sodium hyaluronate 1.4% to form the anterior chamber.
Main Port: Create a trilamellar main port using a 2.2 mm keratome at the 11 o’clock position.
Capsulorhexis: Perform a continuous curvilinear capsulorhexis approximately 5mm in size using Utrata capsulorhexis forceps [Figure 1b]. This size allows for intraocular lens (IOL) implantation in the sulcus with optic capture in case of posterior capsule rupture.[4]
Hydrodelineation: Avoid hydrodissection due to the weak posterior capsule.[1,2] Instead, perform hydrodelineation [Figure 1c] and use viscoelastic (Hydroxypropyl methyl cellulose [HPMC] 2%) to prolapse the soft nucleus (viscodelineation)[1,2] as seen in [Figure 1d]. Once the nucleus floats on a cushion of viscoelastic, it was emulsified using the techniques for phacoemulsification in soft cataracts [Figure 1e], such as the tilt-and-crush[5] or tilt-and-tumble methods.[6]
Anterior chamber Maintenance: Ensure viscoelastic is injected before removing any irrigation source to prevent collapse of the anterior chamber [Figure 1f].
Epinucleus Removal: Use viscodissection[7] to separate the epinucleus from the capsule [Figure 1g], emulsifying and removing it with the phaco probe [Figure 1h]. Form the anterior chamber with 2% HPMC before removing the phaco probe.
Cortex Removal: Remove the cortex [Figure 1i] using bimanual irrigation and aspiration cannulae (I&A). Instead of high vacuum, the aspiration cannula is employed to grasp cortical fibers and separate them through a pulling action. These fibers are then crushed mechanically [Figure 1j] and aspirated. Use viscoelastic generously [Figure 1k] to maintain anterior chamber stability before removing any irrigation sources. Avoid polishing, as this may lead to rupture of the weak posterior capsule. Persistent PPC plaque should be left undisturbed; if it causes visual disturbances, it may be removed later via Nd-Yag Capsulotomy after 2 months.
IOL Implantation: Implant a single-piece, foldable IOL into the capsular bag [Figure 1l], and hydrate the surgical ports. Three piece IOL needs to be kept ready as it may be useful for sulcus implantation in case of posterior capsular rupture.
DISCUSSION
Phacoemulsification cataract surgery is a superior technique for managing posterior polar cataracts (PPC) compared to other methods, such as extracapsular cataract extraction (ECCE), in terms of safety1. While various techniques for phacoemulsification in PPC have been described1,2, there is currently no standard surgical approach to eliminate the primary risks associated with PPC, such as posterior capsular rupture (PCR). The risk of PCR increases when the size of the PPC exceeds 4 mm1. When the nuclear grade is less than 2, nucleus removal or debulking is easy, as the phacoemulsification could be done within the intact posterior epinucleus after hydrodelineation. However, when the nuclear grade exceeds 2, nucleus management requires different techniques depending on the surgeon’s preference and the hardness of the cataract1,2. In our case, since the nucleus is soft and easily prolapsed after hydrodelineation and viscodelineation, we prefer the tilt-and-crush technique5 to emulsify the soft nucleus. If hydrodelineation is not occured, the majority of the nucleus could be emulsified and removed by creating adjacent trenches to form a bowl1, followed by viscodissection to float the remaining matter for emulsification.
CONCLUSION
This case report of a grade II PPC with a soft nucleus demonstrates the essential steps and precautions, illustrated through pictures and video. These insights can be beneficial for ophthalmologists, particularly those who are new or in training, in managing PPCs. When the correct steps are followed, managing a soft nucleus in PPC surgery is simple.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Managing the posterior polar cataract: An update. Indian J Ophthalmol. 2017;65:1350-8.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior polar cataract: A review. Saudi J Ophthalmol. 2012;26:41-9.
- [CrossRef] [PubMed] [Google Scholar]
- Two-Y crushing technique: A simple technique to crack the nucleus in a posterior polar cataract using two-Y rotators. Cureus. 2024;16:e63416.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular lens implantation in the ciliary sulcus: Challenges and risks. Clin Ophthalmol. 2019;13:2317-23.
- [CrossRef] [PubMed] [Google Scholar]
- Tilt-and-crush: A safe, effective and energy-saving technique for soft cataract removal. Eur J Ophthalmol. 2020;30:1162-7.
- [CrossRef] [PubMed] [Google Scholar]
- Tilt and tumble phacoemulsification. Dev Ophthalmol. 2002;34:44-58.
- [CrossRef] [PubMed] [Google Scholar]
- Minimizing risk to the capsule during surgery for posterior polar cataract. J Cataract Refract Surg. 2002;28:742-4.
- [CrossRef] [PubMed] [Google Scholar]






