Translate this page into:
Role of optic zone diameter in scleral lens fitting in traumatic aniridia with scarred cornea – A case report

*Corresponding author: Madhumathi Subramanian, Department of Contact Lens, Sankara Nethralaya, A Unit of Medical Research Foundation, Chennai, Tamil Nadu, India. madhumathi.optom@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Subramanian M. Role of optic zone diameter in scleral lens fitting in traumatic aniridia with scarred cornea – A case report. Lat Am J Ophthalmol. 2024;7:15. doi: 10.25259/LAJO_25_2024
Abstract
Scleral lenses (SLs) are large-diameter rigid gas-permeable lenses that vault over the entire cornea and rest on the bulbar conjunctiva overlying the sclera and maintain a fluid reservoir, which along with the rigidity of the lens masks irregular astigmatism and reduces the aberrations. A 20-year-old male had decreased vision, photophobia, and double vision due to an open globe injury with a shuttle bat 1 year back, followed by which he underwent corneal tear repair and multiple retinal surgeries. He was advised for penetrating keratoplasty elsewhere and came for a second opinion. Based on a diagnostic fitting approach, an 18.5 mm diameter SL was applied on the right eye, with which vision improved from 6/60, N36@ 10 cm to 6/7.5 and reduced the higher-order aberrations but a slightly higher vault was observed. Therefore, a 16.5 mm diameter SL was applied but with this lens, vision decreased to 6/12 with effort, and in both lenses, the patient reported binocular diplopia. Therefore, a combination of management, larger optic zone SLs, and a Fresnel prism was prescribed, which improved the patient’s vision, and reduced diplopia. The purpose of the case report is to emphasize the role of optic zone diameter in SL fitting, particularly in cases of traumatic scarred cornea with eccentric pupils and the importance of co-management.
Keywords
Scleral lenses
Optic zone diameter
Aniridia
Corneal scar
INTRODUCTION
Ocular trauma is often the most common cause of unilateral loss of vision in most developing countries and about 5% of blindness is mostly due to ocular trauma.[1] Corneal scars followed by any ocular injury will result in a significant decrease in vision, glare, haloes, and photophobia due to corneal astigmatism. In fact, in developing countries with a lack of donor material, contact lenses (CLs) are considered the first choice of optical rehabilitation in eyes with a corneal scar following repaired corneal perforation.[2] Corneal lenses are considered to be the first choice of CL management to correct corneal irregularity thus eliminating aniseikonia from unequal prescriptions leading to diplopia.[3,4]
Scleral lenses (SLs) are larger-diameter lenses that create fluid reservoirs, mask irregular astigmatism and reduce glare, haloes, and photophobia by correcting the aberrations and providing good visual quality.[5] This case report explains the management of symptoms like a decrease in vision, glare, and double vision post-traumatic aniridia with a decentered visual axis managed with larger diameter SL and prisms as a temporary resolution.
CASE REPORT
A 20-year-old male presented with complaints of decreased vision, photophobia, and binocular double vision in the right eye, after an open globe injury with a shuttle bat 1 year prior. Based on previous reports, he was diagnosed with a full-thickness corneal tear with iris and vitreous prolapse. For management, silicone oil tamponade, pars plana vitrectomy, pars plana lensectomy, and corneal tear repair have been performed elsewhere. He was advised to undergo penetrating keratoplasty in the right eye and came for a second opinion. On evaluation, the unaided visual acuity in the right eye was 6/60, N36@10 cm, and in the left eye was 6/6 and N6@30– 35 cm. On refraction, there was no further improvement with glasses. A slit-lamp examination revealed partial aniridia with a healed corneal scar, pinguecula, and glued intraocular lens (IOL) in the right eye [Figure 1], and the left eye was within normal limits. Right exotropia (RXT) was noted in the cover test. On pupillary evaluation mid-dilated, an irregular pupil was noted in the right eye. Fundus examination revealed the presence of peripheral laser barrage marks. The patient was referred to the CL clinic for assessment of visual improvement in the right eye. All possible modalities, such as corneal gas-permeable CL, SL, and prosthetic CL, were discussed. Keratometry readings and corneal topography for the right eye were unable to be obtained due to distorted mires and in the left eye K1 was 41.00D@ 180; K2 was 42.00@ 90. A diagnostic fitting approach was followed. An initial trial was performed with rigid gas-permeable lenses and prosthetic CL trials [Table 1]. However, the patient’s vision satisfaction and comfort were poor. Followed by a larger diameter, SL of 18.5mm/3.0Sag/FSE1 trial lens was selected based on the palpebral fissure height and corneal contour of the right eye. Post-insertion fit assessment showed a central clearance of 450 μm and good limbal and haptic alignment with no blanching; however, the lens edge was overriding the pinguecula [Figure 2a] and over-refraction acceptance of −1.00 DS for distance, and vision improved from 6/60 to 6/7.5, and with a near addition of +2.50 DS, vision improved to N6@30–35 cm in primary gaze with fast reading speed. Considering a higher central clearance, a smaller diameter lens of 16.5 mm/2.8 Sag/FSE1 was applied. The lens was impinging the pinguecula [Figure 2b], but the BCVA was 6/12 and was not improving further. The change in lens diameter drastically showed a marked decrease in vision from 6/7.5 to 6/12 with poor reading response, which was due to the difference in optic zone diameter (OZD), especially in this case of the decentered visual axis. I Tracey Aberrometer (Tracy technologies) was performed without and with different SL diameters [Figure 3] to evaluate the change in the visual quality. It was found that root mean square higher order aberration (RMS-HOA) and root mean square (RMSComa) were significantly reduced with large-diameter lenses than with small-diameter lenses. The fit assessment was performed after 3 h and 6 h of lens wear in the 18.5 mm dia trial lens. The patient reported significantly reduced glare and photophobia and was very happy with the significant increase in vision without any eccentric head postures but complained of constant crossed horizontal diplopia. The final SL was ordered with no modification as post 6 h the central clearance was 300 μm, and limbal clearance was 60 μm with no impingement/blanching. The fit assessment was repeated, after which the patient was referred for a Fresnel prism trial over the final lens. A cover test revealed RXT for distance and near. The prism bar cover test for distance and near was 25 prism base-in. In the worth four dot test, crossed diplopia was present for distance and near. A prism trial with 20 prism base-in was done over the final CL in the right eye, with the prism patient reported a fusion of images with very minimal wobbling of images. The Fresnel prism was prescribed with a proper explanation as temporary relief from diplopia, as the patient was not willing to undergo surgical intervention. One year after the initiation of SL, vision, and fit were the same, but the patient was willing to undergo squint correction at the current visit. Post-squint correction, diplopia was reduced and vision with SL was the same, and the patient was even more comfortable.
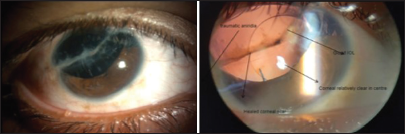
- Slit-lamp photograph of traumatic partial aniridia with scarred cornea.
| Lens | Rigid lens | Prosthetic type C |
|---|---|---|
| Base curve | 7.85 | 8.6 |
| Power | −3.00 DS | Plano |
| Diameter | 9.50 mm | 14.00 mm (10.5 mmiris diameter) |
| Over refraction | +1.00 DS | +4.00 DS |
| Vision | 6/9 with a lot of effort | 6/12 |
| Fit Assessment | Irregular Fluorescein pattern with decentered lenses | Ideal |
| Patient comfort | Poor, No comfort, and diplopia | Poor, No vision improvement, diplopia but reduced photophobia |
DS: Diopter Sphere
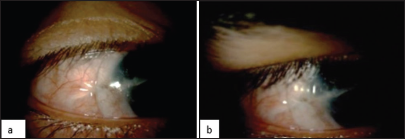
- (a) 16.5 mm diameter scleral lenses (SL) impinging on the pinguecula and (b) 18.5 mm diameter SL impinging on the pinguecula.
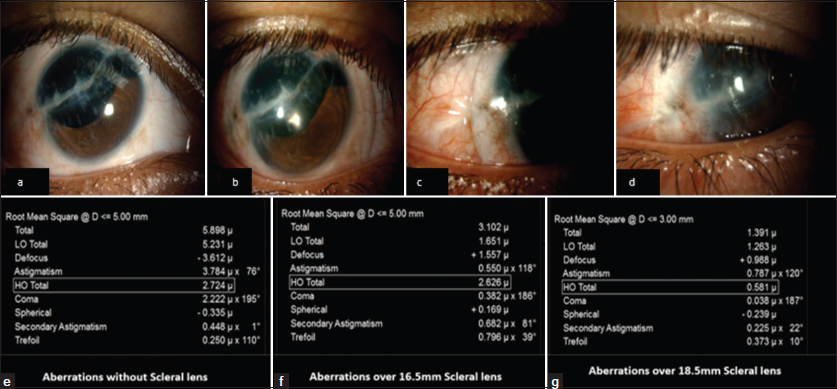
- Aberrations with and without scleral lens. (a) Traumatic aniridia with corneal scar, (b) Eye fitted with 16.5 mm scleral lens, (c) Eye fitted with 16.5 mm scleral lens resting on pinguecula, (d) 18.5 mm scleral lens covering the pinguecula, (e) Aberrations without scleral lens, (f) Aberrations over 16.6 mm scleral lens, (g) Aberrations over 18.5 mm scleral lens.
DISCUSSION
The present case report highlights the importance of OZD in cases of decentered visual axis. The role of CL in improving visual performance has been thoroughly established over the years. Studies have provided clear evidence that correcting mild and moderate irregular corneal conditions using conventional gas permeable lenses will help in the enhancement of visual performance such as spatial vision, depth perception, and optical performance (higher order aberration), and in case of advanced conditions, rose K and SLs may require.[6-8] Fitting corneal gas permeable lenses in advanced conditions can be challenging as it can result in lens decentration, dislocation, or discomfort. When comparing the benefits of SL over the corneal gas permeable lenses for advanced corneal conditions, SL achieves greater comfort, centration, and stability, and provides good visual outcomes and long-term safety and efficacy.[6-8] In addition, this case report highlights that choosing the optimal lens diameter in SL fitting also plays a key role in achieving better comfort and vision. Hence, not only the vault and haptic portion of the scleral are important during SL fitting but even the OZD which comprises the refractive error also plays a key role in better visual performance in the decentered visual axis.
Corneal rigid lenses would induce a vertical prismatic imbalance due to inferior lens decentration, especially in cases of irregular corneas leading to diplopia and unstable vision. SLs are larger diameter lenses which by increasing the lens stability and increased lens thickness reduce the prismatic effects.[9]
It is reported that up to 5 Prism diopters can be incorporated into the SL by customizing the anterior SL profile.[10] A few cases reported by Bragg and Sindt and Frogozo found that the use of prism incorporation into the SL has eliminated the intermittent vertical and horizontal diplopia in cases of high myopia and presbyopia and also in cases of bilateral radial keratotomy.[9,11] In the current case due to a lack of technology for prism incorporation in SL, a Fresnel prism glasses over the SL were prescribed as an ideal option until the surgical procedure.
CONCLUSION
This case report explains the management of symptoms like a decrease in vision, glare, and double vision post-traumatic aniridia with a decentered visual axis managed with larger diameter SLs and prisms as a temporary resolution when advanced technology of incorporating a prism in SL is not available.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Contact lens rehabilitation following repaired corneal perforations. BMC Ophthalmol. 2006;6:11.
- [CrossRef] [PubMed] [Google Scholar]
- Rigid gas permeable contact lens for visual rehabilitation in aphakia following trauma. Clin Exp Optom. 2012;95:499-505.
- [CrossRef] [PubMed] [Google Scholar]
- Visual rehabilitation with contact lenses after ocular trauma. Arq Bras Oftalmol. 2008;71:23-31.
- [CrossRef] [PubMed] [Google Scholar]
- A guide to scleral lens fitting, Version 2.0 Forest Grove, OR: Pacific University; 2015. p. :44-51. Ch. 5
- [Google Scholar]
- Potential contraindications to scleral lens wear. Contact Lens Anterior Eye. 2019;42:92-103.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of scleral lenses on vision, refraction and aberrations in post-LASIK ectasia, keratoconus and pellucid marginal degeneration. Ophthalmic Physiol Opt. 2021;41:664-72.
- [CrossRef] [PubMed] [Google Scholar]
- Objective and subjective performance of scleral lenses and new advances in scleral lens technologies Netherlands: Utrecht University; 2015.
- [Google Scholar]
- Correction of binocular diplopia with novel contact lens technology. J AAPOS. 2015;19:e38.
- [CrossRef] [Google Scholar]
- Optical considerations for scleral contact lenses: A review. Contact Lens Anterior Eye. 2019;42:598-613.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of horizontal diplopia with prism correction in scleral gas permeable prosthetic device In: Global specialty lens symposium. 2016.
- [Google Scholar]






