Translate this page into:
Ultrasound biomicroscopy evaluation of pseudophakic pupillary block by vitreous prolapse after Nd:YAG laser posterior capsulotomy

*Corresponding author: Agustín Nicolás Lucas, Departments of Glaucoma, Hospital Oftalmológico Dr. Pedro Lagleyze, Juan B. Justo 4151, CABA - 1212, CABA, Argentina. aguslucas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Lucas AN, Pedalino A, Anauati AP, Catalano C. Ultrasound biomicroscopy evaluation of pseudophakic pupillary block by vitreous prolapse after Nd:YAG laser posterior capsulotomy. Lat Am J Ophthalmol 2020;3:5.
Abstract
Intraocular pressure rise is a common complication after neodymium:yttrium-aluminum-garnet (Nd-YAG) laser posterior capsulotomy. Although in most cases it is related to an inflammatory response, there are other possible mechanisms such as misdirection syndrome and pupillary block. The authors report two cases of pupillary block by vitreous prolapse after Nd-YAG laser posterior capsulotomy evaluated by ultrasound biomicroscopy (UBM). UBM allows to differentiate possible causes of intraocular pressure rising after laser capsulotomy even in cases of corneal opacity. It also allows to detect intraocular lens dislocation, sometimes associated with this situation. This is the first report that describes the characteristics of UBM images of this complication.
Keywords
Glaucoma
Angle closure/etiology
Laser therapy
Eye Diseases/complications
Acute disease
Anterior eye segment/Diagnostic imaging
INTRODUCTION
Posterior capsule opacification is the most frequent late complication of cataract surgery.[1] Neodymium:yttrium-aluminum-garnet (Nd-YAG) laser capsulotomy is considered the elective treatment. Despite being a non-invasive low-risk intervention, it is not exempt of complications. Intraocular lens (IOL) pitting, iritis, and rise of intraocular pressure (IOP) are the most frequent complications.[2]
The possible causes of IOP rise are an inflammatory crisis,[2] misdirection syndrome,[3,4] and pupillary block. Acute angle closure by pupillary block in pseudophakic patients is a rare complication and only few cases have been reported. The blocking mechanism is attributed to vitreous prolapse with[5] or without IOL dislocation.[6,7] The aim of this report is to present two cases of pupillary block by vitreous prolapse after Nd:YAG laser posterior capsulotomy that has been evaluated both by slit-lamp and ultrasound biomicroscopy (UBM). This is the first report that describes the characteristics of UBM images of this complication.
CASE REPORT
Case 1
An 80-year-old female presented a history of uncomplicated extracapsular cataract surgery in the right eye (OD) 15 years ago and uncomplicated phacoemulsification cataract surgery in the left eye (OS) 10 years ago. When capsular opacity was noted, Nd-YAG laser posterior capsulotomy was performed in both eyes. Twenty-four hours later, she arrived to the emergency room suffering from ocular pain and decrease in visual acuity in OD.
Ophthalmological examination revealed a visual acuity of 20/400 OD and 20/40 OS. The right eye presented a narrow chamber compared to the left one, severe corneal edema, and intermediate non-reactive mydriasis. The left eye did not present any particularity. IOP was 60 mmHg in the right eye and 16 mmHg in the left one. The patient was treated with a combination of 2% dorzolamide-0.5% timolol b.i.d., 1% prednisolone acetate q.i.d., and acetazolamide 250 mg q.i.d.
UBM (Sonomed VuMAX™ II UBM) was performed [Figures 1 and 2], detecting a closed angle 360º with pupillary block configuration. Both optic and haptics of the IOL were placed in sulcus with no sign of dislocation. There was no evidence of any element blocking the pupil and an anechoic space between the pupil and the IOL was present. Ciliary bodies were not placed anteriorly.
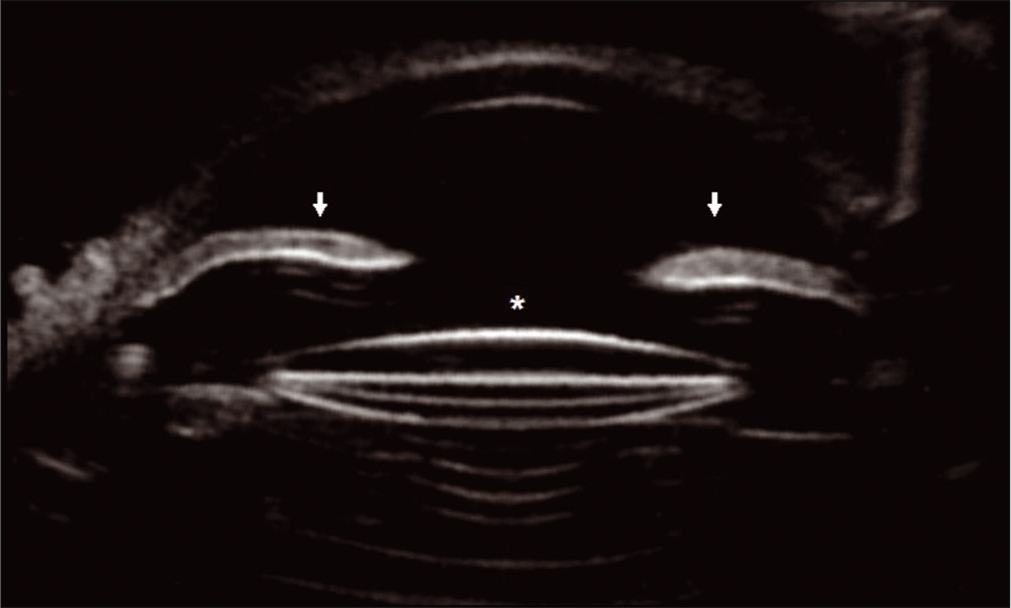
- Case 1: Iris anterior convexity (arrows) characteristic of pupillary block. No structure is observed obstructing the pupil and there is an anechoic space between the iris and the Intraocular lens (IOL) (asterisk). Both IOL optic and haptics are placed in sulcus.

- Case 1: Angle detail: Closed angle (arrow), iris anterior convexity and haptic located in sulcus (arrowhead).
After the instillation of a drop of 10% glycerin, better visualization of the anterior segment was achieved and a peripheral iridotomy with Nd-YAG laser was performed. At that moment, the presence of vitreous coming through the iridotomy was noticed. The IOP did not reduce and the narrow chamber and non-reactive pupil persisted. An anterior vitrectomy was performed 24 h later. After the surgery, the pupil became reactive and the IOP started to decrease.
At present, her IOP ranges between 12 and 16 mmHg in both eyes without medication and her visual acuity is 20/30 OD and 20/20 OS.
Case 2
A 67-year-old male presented a history of uncomplicated phacoemulsification cataract surgery in OS 4 years ago. A Nd-YAG laser posterior capsulotomy was performed in the left eye and 60 days later, he was evaluated on an urgent basis for acute ocular pain and a decrease in his visual acuity in the left eye of 72 h of evolution.
Ophthalmological examination revealed a visual acuity of 20/30 OD and 20/200 OS. The left eye presented a narrow chamber, mild corneal edema, and intermediate non-reactive mydriasis. The right eye did not present any particularity, but showed a wide chamber instead. Intraocular pressure was 18 mmHg OD and 46 mmHg OS. The patient was treated with a combination of 2% dorzolamide-0.5% timolol b.i.d., 1% prednisolone acetate q.i.d., and acetazolamide 250 mg q.i.d.
Suspecting an acute angle closure, a peripheral iridotomy with Nd-YAG laser was performed. The IOP decreased and the anterior chamber widened considerably.
UBM (Sonomed VuMAX™ II UBM) was performed [Figure 3], detecting vitreous prolapse blocking the pupil. Both optic and haptics of the IOL were placed inside the capsular bag with no sign of dislocation. The peripheral iridotomy showed permeable, whereas the angle was open in some degrees, it showed closed in others, probably caused by peripheral anterior synechiae.

- Case 2: After iridotomy was performed, the iris presents a flattened position. Vitreous prolapse is observed obstructing the pupil (arrow). Both intraocular lens optic and haptics are placed inside the capsular bag.
At present, his IOP ranges oscillate between 18 and 20 mmHg in both eyes without medication and has a visual acuity of 20/30 OD and 20/40 OS.
DISCUSSION
Pupillary block is a highly infrequent complication of Nd- YAG laser posterior capsulotomy in pseudophakic patients. It may occur immediately after the procedure or time after. When it happens inmediately after, it is important to establish a differential diagnosis from inflammatory IOP rising and misdirection syndrome. The acute increase on IOP measurements is usually associated with corneal edema that complicates slit-lamp evaluation. In these cases, UBM becomes of utility to confirm pupillary block configuration.[8]
In cases of inflammatory IOP rising, the IOP values are lower than in the differential diagnosis and UBM shows wide chambers with open angles and flat iris. Misdirection syndrome, however, presents shallow anterior chambers with anterior rotation of ciliary bodies and IOL displaced anteriorly.[9,10] Pupillary blocks are associated with narrow chambers, close angles, and iridian anterior convexity.[11]
Pupillary block by vitreous prolapse may or may not be associated with IOL dislocation. UBM shows the exact position of both optic and haptics and their relation with other structures. It is important to take IOL location into consideration given the fact that, in cases of dislocation, removal of the IOL along with vitrectomy is suggested.[5]
Vitreous humor is shown anechoic in UBM, with an echogenicity similar to aqueous humor, and it is not always possible to detect it.[12] When pigment or inflammatory particles are attached to vitreous face, its detection becomes possible. In Case 2, the presence of particles allows the detection of the vitreous face as hyperechogenic. This process generally indicates a longer evolution. The presence of pupillary block configuration where there are no visible elements blocking the pupil and there is an anechoic space between iris and IOL, as in Case 1, is highly suggestive of pupillary block by vitreous prolapse.
There is no standardized treatment for this complication. We suggest peripheral iridotomy in a first instance and surgical intervention in case of refractoriness.
CONCLUSION
Pupillary block by vitreous prolapse after Nd-YAG laser posterior capsulotomy is a rare and severe complication that can compromise the patient’s visual acuity. UBM allows to establish an early diagnosis even in cases of corneal opacity. It is useful to differentiate causes of IOP rising after capsulotomy and to detect IOL position. In case of confirmation of pupillary block by vitreous prolapse, we recommend peripheral iridotomy in first instance, followed by surgical intervention, if the problem is not solved by the former.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Posterior capsule opacification: A cell biological perspective. Exp Eye Res. 2002;74:337-47.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of Nd:YAG laser capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3:45-50.
- [Google Scholar]
- Aqueous misdirection syndrome: A complication of neodymium: YAG posterior capsulotomy. J Cataract Refract Surg. 1994;20:563-5.
- [CrossRef] [Google Scholar]
- Malignant glaucoma as a complication of Nd:YAG laser posterior capsulotomy. Ophthalmic Surg Lasers Imaging. 2004;35:248-50.
- [CrossRef] [Google Scholar]
- Spontaneous posterior dislocation of an intraocular lens presenting as pupillary block glaucoma. J Cataract Refract Surg. 2000;29:410-1.
- [CrossRef] [Google Scholar]
- Acute angle-closure glaucoma caused by vitreous prolapse after neodymium:YAG posterior capsulotomy. J Cataract Refract Surg. 2004;30:2445-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pupillary block glaucoma secondary to vitreous prolapse after Nd:YAG capsulotomy. Clin Exp Optom. 2011;94:383-4.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound biomicroscopy. High-frequency ultrasound imaging of the eye at microscopic resolution. Radiol Clin North Am. 1998;36:1047-58.
- [CrossRef] [Google Scholar]
- Malignant glaucoma. Clinical and ultrasound biomicroscopic features. Ophthalmology. 1994;101:1030-5.
- [CrossRef] [Google Scholar]
- Ultrasound biomicroscopy in pseudophakic malignant glaucoma. Ophtalmology. 1993;100:1330-4.
- [CrossRef] [Google Scholar]
- Ultrasound biomicroscopy of anterior segment structures in normal and glaucomatous eyes. Am J Ophthalmol. 1992;113:381-9.
- [CrossRef] [Google Scholar]
- Ultrasonic evaluation of the vitreous and retina. Semin Ophthalmol. 1998;13:210-8.
- [CrossRef] [PubMed] [Google Scholar]






