Translate this page into:
Application of cyanoacrylate glue in corneal impending perforation (descemetocele) under slit lamp biomicroscope

*Corresponding author: Balamurugan Ramatchandirane, Department of Ophthalmology, All India Institute of Medical Sciences, Mangalagiri, Andhra Pradesh, India. bala16690@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Ramatchandirane B, Patil GR, Devalla MD. Application of cyanoacrylate glue in corneal impending perforation (descemetocele) under slit lamp biomicroscope. Lat Am J Ophthalmol. 2025;8:5. doi: 10.25259/LAJO_31_2024
Abstract
A male in his sixties had been treated outside initially as right eye suspected viral stromal keratitis with oral acyclovir and topical prednisolone 1% and later as suspected microsporidial stromal keratitis with oral albendazole, topical voriconazole 1% and topical prednisolone 1%. In our management, we have ruled out microsporidia by corneal scraping, restarted antiviral treatment, and stopped topical prednisolone in view of the epithelial defect. The patient slowly improved with the complete disappearance of the infiltrates, but there was a persistent epithelial defect that turned into a descemetocele. Hence, we have performed cyanoacrylate glue application on the descemetocele under a slit lamp biomicroscope in outpatient department (OPD) settings. In this case report, we have demonstrated and educated the important steps and precautions in the corneal tissue adhesive glue application under a slit lamp biomicroscope in OPD settings.
Keywords
Cyanoacrylate glue
Descemetocele
Impending corneal perforations
Outpatient department settings
Slit lamp guidance
INTRODUCTION
A male in his sixties had initially been treated outside for suspected viral stromal keratitis of the right eye with oral acyclovir and topical prednisolone 1%. He was later treated for suspected microsporidial stromal keratitis with oral albendazole, topical voriconazole 1%, and topical prednisolone 1%. Upon presentation, there was necrotizing stromal keratitis approximately 4 mm × 4 mm in size [Figure 1a]. We ruled out microsporidia by corneal scraping and restarted antiviral treatment, discontinuing topical prednisolone due to the epithelial defect. The patient slowly improved with the complete disappearance of the infiltrates, but a persistent epithelial defect [Figure 1b] developed into a descemetocele [Figure 1c and d] of approximately 0.5 mm. Consequently, we performed cyanoacrylate glue application on the descemetocele[1,2] under a slit lamp biomicroscope in an outpatient setting. In this case report, we aim to demonstrate and educate on the important steps and precautions for corneal tissue adhesive glue application under a slit lamp biomicroscope in outpatient settings.
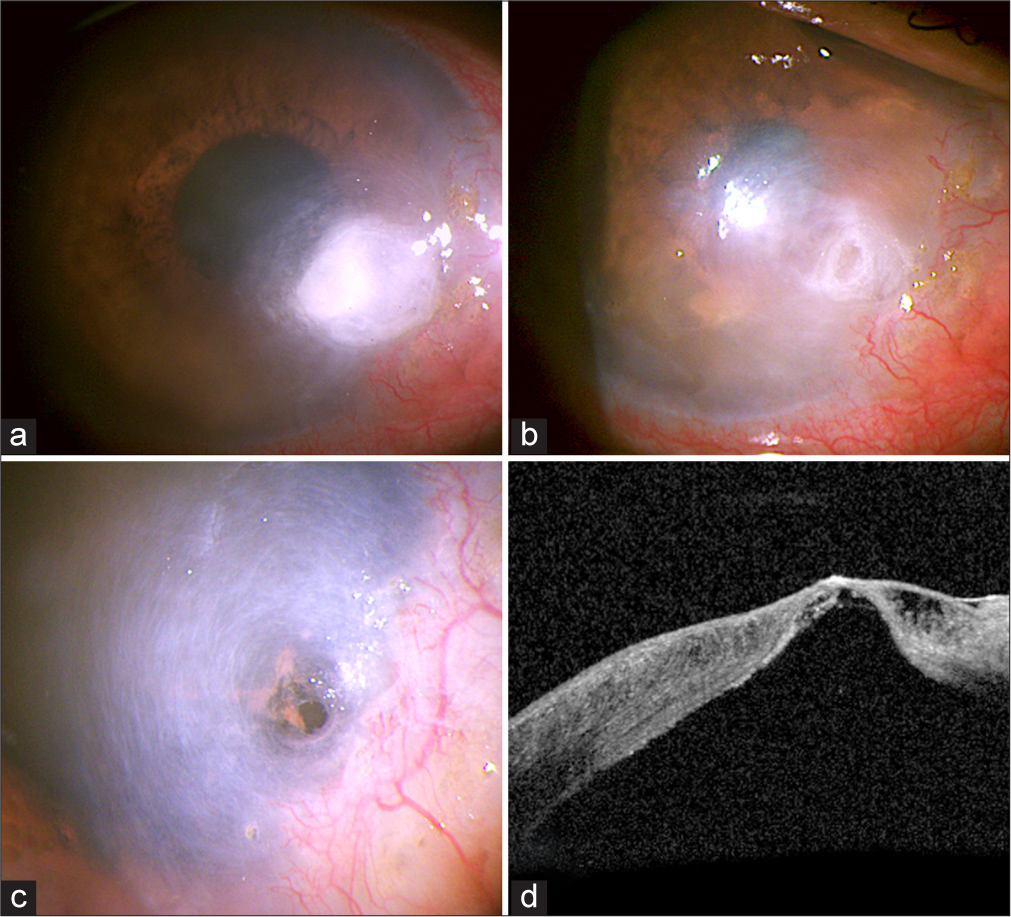
- (a) Showing dense corneal stromal infiltrates approximately 4 mm × 4 mm in size. (b) showing the formation of the epithelial defect after 14 days of antimicrobial treatment. (c) illustrating the bulging of Descemet’s membrane, indicating a descemetocele (impending corneal perforation). (d) showing the anterior segment-optical coherence tomography (OCT) image of the descemetocele.
Important steps for corneal glue application under a slit lamp biomicroscope
Preparation of necessary materials[1,2] included topical anesthesia (proparacaine 0.5%), N-butyl cyanoacrylate glue, a bandage contact lens (BCL), and sterile instruments such as plain forceps, a wire eye speculum, a cotton tip applicator, a 26G needle, and 1CC and 2 CC syringes, as shown in [Figure 2].
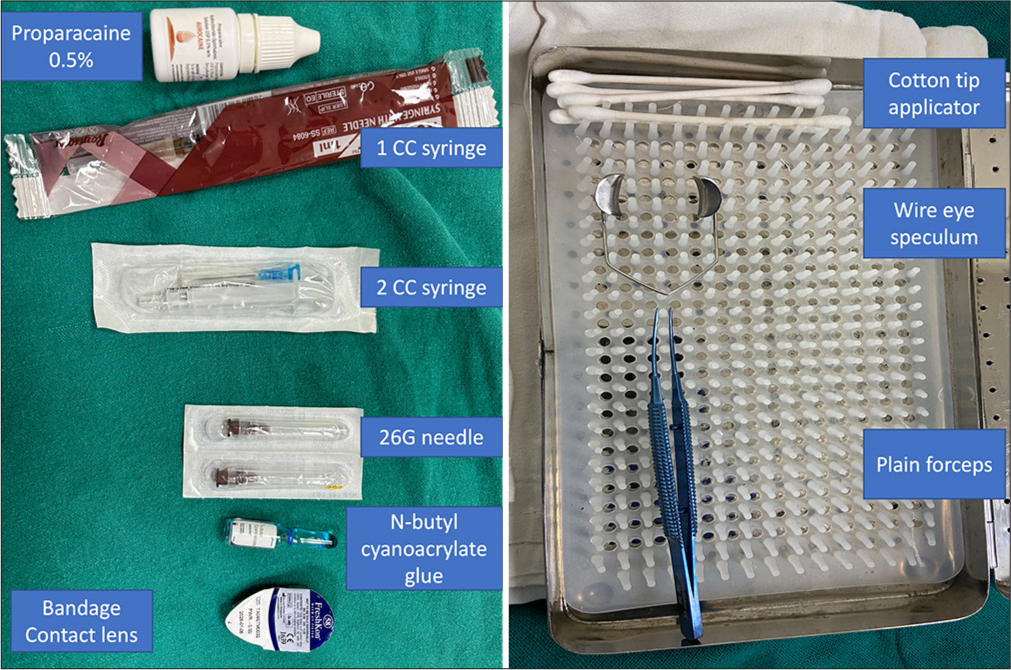
- Important materials needed for glue application such as N-butyl cyanoacrylate glue, a bandage contact lens, proparacaine 0.5%, and sterile instruments like a wire eye speculum, plain forceps, and a cotton tip applicator.
The important steps [Video 1] consist of:
Video 1:
Video 1:The application of cyanoacrylate glue in corneal impending perforation (descemetocele) under slit lamp biomicroscope video is accessible from the portal.-
Careful application of the wire speculum without exerting undue pressure on the globe [Figure 3a]. Undue pressure during corneal application can lead to perforation.
Taking an appropriate amount of glue at the 26G needle tip beforehand, then approaching the cornea for application [Figure 3b], using a cotton tip applicator for quick solidification of the glue [Figure 3c], and supplementing the glue application based on the clinical situation.
Application of the BCL [Figure 3d].
Careful removal of the wire speculum without applying undue pressure to the eye globe.
After application, anterior segment optical coherence tomography (AS-OCT) was repeated, showing the BCL and glue in place [Figure 3e and f]. The patient was given prophylactic antibiotics (moxifloxacin 0.5%) 4 times a day. At 30 days, the glue was intact with active invasion of corneal vessels [Figure 3g]. There were no signs of infection, and the BCL was changed at this time.
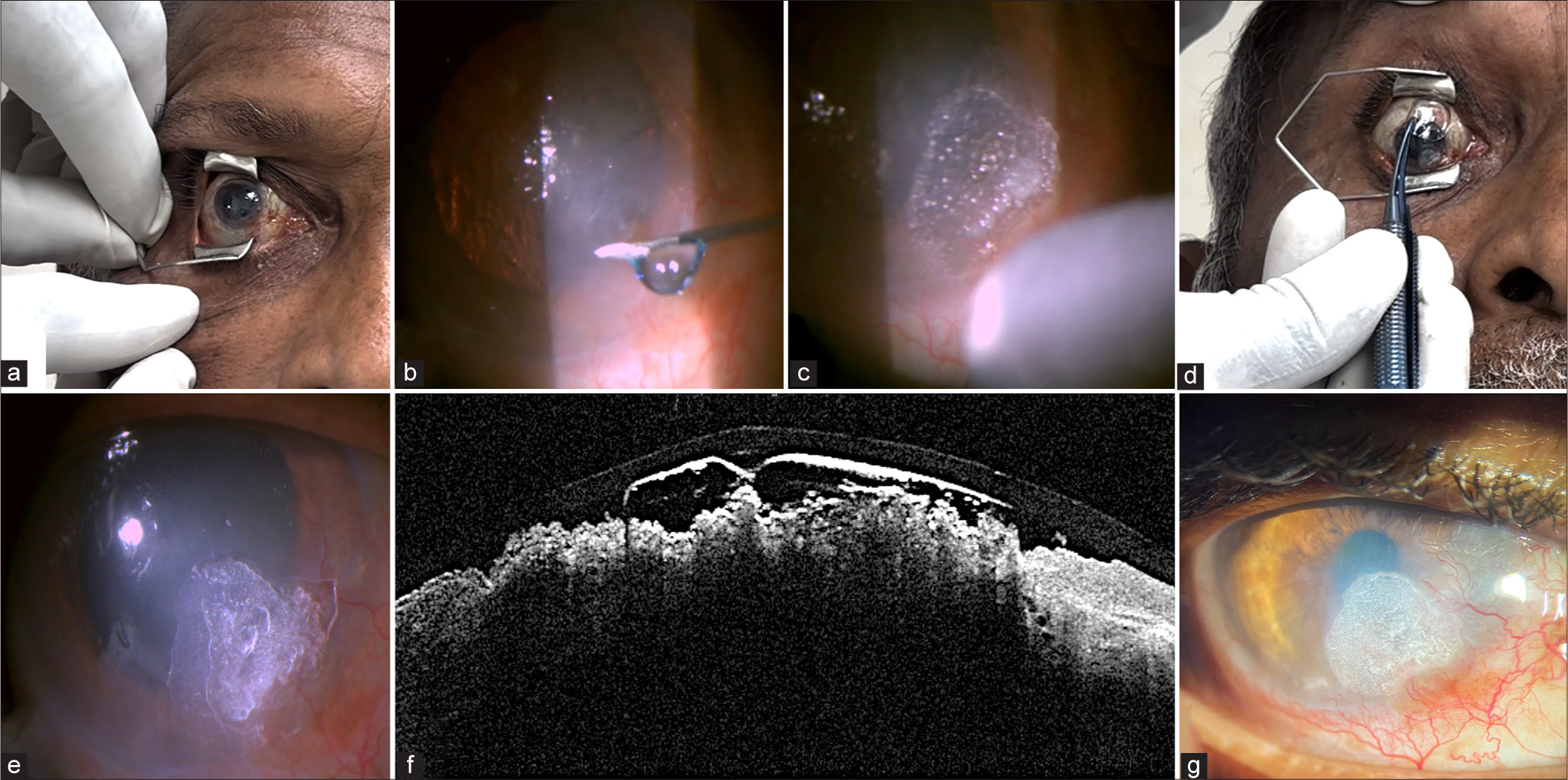
- (a) Demonstrates the careful application of the wire eye speculum without undue pressure on the globe. (b) showing a 26 G needle with the appropriate amount of glue taken at the needle tip beforehand, then applied to the descemetocele. (c) illustrating the quick solidification of the glue after application with a cotton tip applicator. (d) showing the application of the bandage contact lens (BCL). (e) presenting the immediate post-operative image of the glue in place with the BCL, (f) confirmed by anterior segment-optical coherence tomography . (g) showing the well-intact glue with the active invasion of blood vessels 30-day post-glue application.
DISCUSSION
Small corneal perforations (less than 3 mm) or descemetoceles often require the use of tissue adhesive to seal the defect. N-butyl cyanoacrylate, a synthetic tissue adhesive, is commonly used for this purpose.[1,2] It is an ester derivative of cyanoacrylic acid monomers, which rapidly polymerizes in the presence of anions found in organic tissue, forming a stable barrier across the defect. This adhesive can be applied in an outpatient department (OPD) setting under a slit lamp, provided there is no significant leakage of aqueous humor. The procedure is quick, inexpensive, and convenient for both the patient and the ophthalmologist. However, if there is substantial aqueous humor leakage or if iris tissue is plugging the defect, the application should be performed in an operating theatre under operating microscope.[1,2]
CONCLUSION
This case report highlights the preparations and important steps for cyanoacrylate glue application under slit lamp guidance in outpatient settings. Although the steps, such as eye speculum application, are straightforward, care must be taken to avoid undue pressure on the globe, which may lead to perforation. Slit lamp-assisted tissue adhesive glue application in cases of impending corneal perforation is simple, reducing operating theater charges while yielding promising results. However, in the case of perforated corneal ulcer, the application of cyanoacrylate glue is preferable to be done under operation theater settings.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Management of descemetocele: Our experience and a simplified treatment algorithm. Indian J Ophthalmol. 2022;70:1564-70.
- [CrossRef] [PubMed] [Google Scholar]
- Management of corneal perforations in dry eye disease: Preferred practice pattern guidelines. Indian J Ophthalmol. 2023;71:1373-81.
- [CrossRef] [PubMed] [Google Scholar]






